The Implications of Obesity on Total Hip Arthroplasties: A Literature Review of the Associated Complications
Ryan P. Bialaszewski1*, Robert H. Ablove2
1University of Texas Rio Grande Valley, School of Medicine, Edinburg, TX, USA
2UBMD Department of Orthopaedics and Sports Medicine, Jacobs School of Medicine and Biomedical Sciences, State University of New York at Buffalo, Buffalo, NY, USA
Abstract
Introduction: Obesity is a global pandemic and public health crisis associated with a wide range of comorbidities, including osteoarthritis, leading to a significantly younger age at the time of primary total hip arthroplasty (THA) and an increased rate of complications compared to nonobese individuals. As our population continues to get older, combined with an increasing rate of obesity, an increased rate of consultations for total hip arthroplasty is expected. This has led to concerns regarding the implications of obesity on the need for THA itself and the associated complications, especially for arthroplasty surgeons. Unfortunately, few articles provide an all-encompassing review of different complications surrounding obesity within orthopedic surgery, and even fewer around total hip arthroplasty. This literature review aims to provide a comprehensive review of the implications obesity has on total hip arthroplasties, its associated complications, and how we can potentially modify these risks.
Methods: Sources and research articles were identified by searching the databases of PubMed, Google Scholar, and the National Center for Biotechnology Information (NCBI) from 2000 to July 2022. Our search used the specific terms located within the abstract/title, including: “total hip arthroplasty” AND “complications,” AND “obesity, OR obese.” Inclusion criteria for research articles were the English language and peer-reviewed articles published from inception to July 2022. Articles not directly examining the effect of obesity on the incidence of complications following primary THA were excluded. Studies with outcomes of interest included the incidence of postoperative complications, primary THA in obese patients, and clinical outcome measures. A total of 265 studies were identified upon initial search. Thirty-one articles were selected for reference in this literature review.
Results: Obese patients undergo primary THA at an earlier age and experience an increased duration of surgery, higher rates of infection, dislocation, periprosthetic fractures, and venous thromboembolism compared to nonobese patients. The role of pre-operative bariatric surgery before total hip arthroplasty has failed to show reductions in complication rates. Harris Hip Scores are lower in obese patients pre-operatively and post-operatively, but the degree of improvement following THA is similar compared to nonobese patients. Long-term survival of total hip prostheses is similar when compared to nonobese patients.
Conclusion: Current literature strongly suggests increased complication rates in obese patients who undergo THA. This phenomenon is not solely due to biomechanical forces and is multifactorial, including inflammatory and genetic predispositions, which need further study. The decision to perform THA on obese patients should not solely be based on BMI. Other factors, such as management of comorbidities, surgical exposure, and nursing care, should be considered when deciding on surgical candidacy.
Introduction
Obesity is a global pandemic and public health crisis with a prevalence that has tripled since 1975 and a current estimation of 650 million adults suffering from obesity worldwide1. Medical costs of obesity in the United States were nearly $173 billion in 2019, accounting for approximately $1,861 higher medical costs annually in obese adults compared to people of healthy weight2. The definition of 'obesity' is a body mass index (BMI) ≥ 30 kg/m2, with 'severe obesity' characterized as a BMI≥ 35 kg/m2 and 'morbid obesity' defined as a BMI ≥ 40 kg/m2.3
Osteoarthritis (OA) of the hip is a degenerative disease; causing disability, pain, and loss of function5. OA is considered a multifactorial disease and increases in prevalence with concurrent obesity, advanced age, female gender, low socioeconomic status, and genetics6. Although there has yet to be a precise relationship between obesity and osteoarthritis, the two conditions are strongly correlated, and the etiology is believed to be biomechanical, proinflammatory, and immunomodulatory6. Obesity is associated with a wide range of comorbidities, including osteoarthritis, leading to a significantly younger age at the time of primary total hip arthroplasty (THA) compared to nonobese individuals4. As our population continues to get older, combined with an increasing rate of obesity, an increased rate of consultations for total hip arthroplasty is expected.
This has led to concerns regarding the implications of obesity on the need for THA itself and the associated complications, especially for arthroplasty surgeons. Unfortunately, few articles provide an all-encompassing review of different complications surrounding obesity within orthopedic surgery, and even fewer specifically address complications associated with total hip arthroplasty. This literature review aims to provide a comprehensive review of the implications obesity has on total hip arthroplasties, its associated complications, and how we can potentially modify these risks.
Methods and Materials
Sources and research articles were identified by searching the databases of PubMed, Google Scholar, and the National Center for Biotechnology Information (NCBI) from 2000 to July 2022. Our search used the specific terms located within the abstract/title, including: “total hip arthroplasty” AND “complications,” AND “obesity, OR obese.” Inclusion criteria for research articles were the English language and peer-reviewed articles that were either observational studies, randomized controlled trials, systematic reviews, literature reviews, or meta-analyses published from inception to July 2022. Articles not directly examining the effect of obesity on the incidence of complications following primary THA were excluded. The first author (RB) performed study selection and data analysis unblinded. Multiple reviewers did not independently assess the articles, and inter-rater reliability was also not evaluated. Studies with outcomes of interest included the incidence of postoperative complications, primary THA in obese patients, and clinical outcome measures. A total of 265 studies were identified upon initial search. After reviewing abstracts, removing articles that met exclusion criteria, and removing duplicate articles, 58 remained under consideration. Full-text articles were then read, and 31 articles were selected for reference in this literature review. A PRISMA flow diagram was not created for this literature review.
Results
Age at primary THA
Four studies directly examined the degree of obesity on the timing of primary THA, which showed a clear inverse relationship between the two variables4,7-9. Abdulla et al. analyzed 10,902 total hip arthroplasty, noting patients with a BMI of 30 kg/m2 or greater required a THA 1.7 years earlier than patients of normal weight (65.4 vs. 67.1). Patients with a BMI of 35 kg/m2 or greater required a THA 3.4 years earlier (63.7 vs. 67.1), and patients with BMI was 40 kg/m2 or greater required a THA 5.8 years earlier (61.3 vs. 67.1) (p-value < 0.001)7. Haynes et al. also identified an earlier age of THAs in obese patients4. Andrew et al. retrospectively reviewed 1421 patients undergoing primary THA and noted mean age of patients at the time of surgery in nonobese, obese, and morbidly obese groups were 69.1 years (21.3 to 94.9), 65.5 years (33.4 to 86.9), and 60.6 years (28.5 to 78.0) respectively (analysis of variance (ANOVA), p < 0.001)8. Lübbeke et al. found patients with a BMI < 30kg/m2 were nearly a mean two years older at the time of THA compared to patients with a BMI > 30 kg/m2 (69.0 versus 67.2 years of age, respectively)9 (Figure 1).
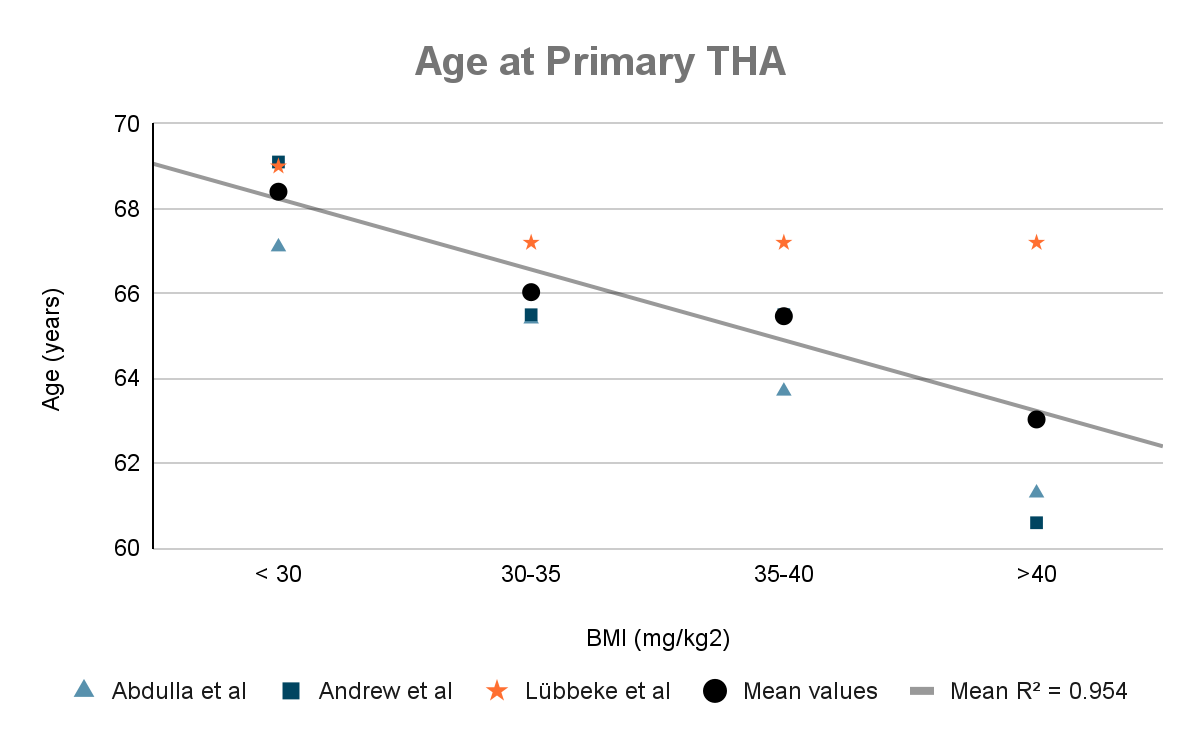
Figure 1: Summarization of the inverse relationship between BMI and age at primary THA described by Abdulla et al., Andrew et al., and Lübbeke et al. (Lübbeke et al. only differentiated between BMI > 30 and < 30)7-9
Duration of surgery
The impact of obesity on operative time is crucial to understand for surgeons optimizing patient care and resource allocation. A meta-analysis that included seven studies totaling 2608 hips by Liu et al. showed a positive correlation between degrees of obesity and operative time. Specifically, obese patients with a BMI greater than 30 kg/m2 experienced a mean deviation of 10.67 minutes longer operative time than patients with a BMI less than 30 kg/m2 (95% CI [3.00, 18.35], p = 0.005). When performing a subgroup analysis of these operative times, for those with a BMI greater than 40 kg/m2, the mean operative time was 37.6 minutes longer when compared to patients with a BMI less than 30 kg/m2 (p < 0.0001)10. However, in Liu et al.'s meta-analysis, it was found that out of the seven studies compared, six exhibited non-significance with 95% confidence intervals, as indicated by negative lower bounds. Figure 2 demonstrates the positive correlation between operative time and BMI to enhance the clarity and visual representation of these results.
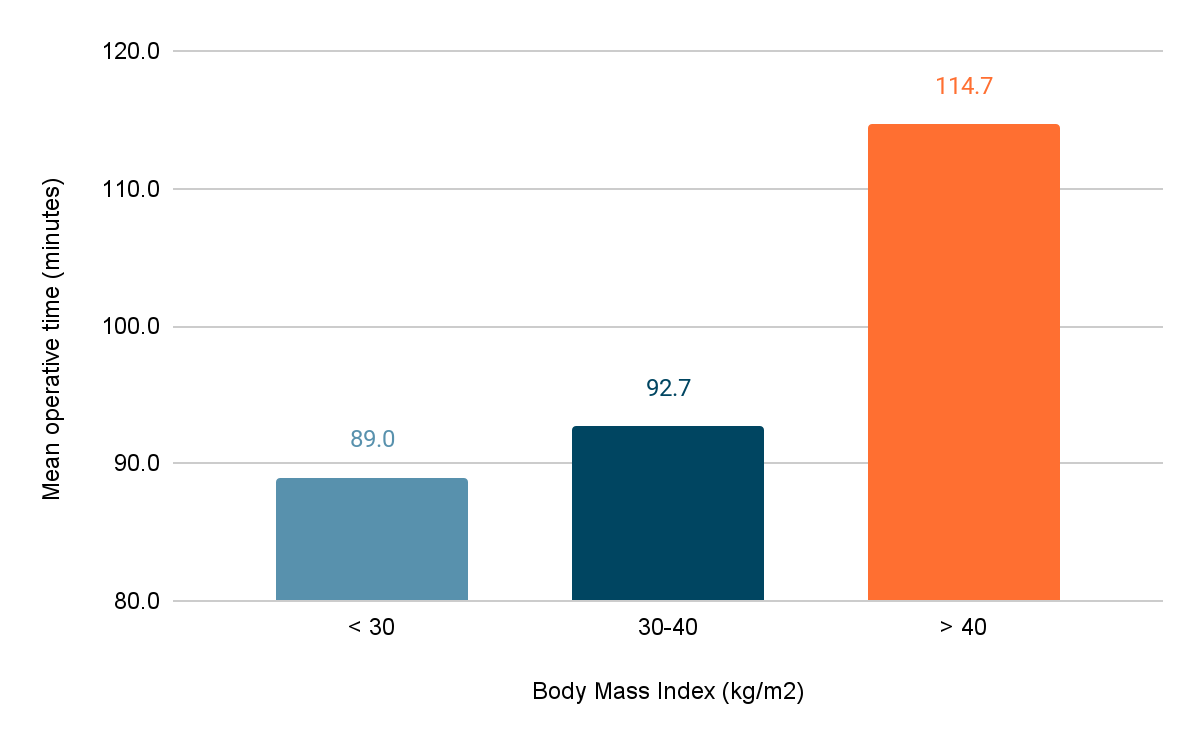
Figure 2: A positive correlation exists when comparing average primary THA operative times to increasing degrees of BMI reported by Liu et al. Subgroup analysis showed BMI 30-40 kg/m2 vs. BMI < 30 kg/m2 had a mean difference of 3.74 minutes, 95% CI [1.12, 6.36], and BMI > 40 kg/m2 vs. BMI < 30 kg/m2 had a mean difference of 37.6 minutes 95% CI [22.99, 52.19]10
Complications
Infection
The association between total hip arthroplasty in obese patients and surgical wound/prosthetic joint infections has been supported by several studies10-14. When stratified, this data shows increased infection rates in higher BMI categories of > 40 and > 50 kg/m2 compared to other obese categories11,12. Onggo et al. performed a meta-analysis including more than 2 million patients. In this meta-analysis, obese patients were found to have a higher risk of deep infections (OR = 2.71, P < 0.001) and superficial infections (OR = 1.99, P < 0.001) when compared to nonobese patients13. Additionally, Liu et al. identified a relative risk of 2.92 for obese patients to develop a deep infection following THA compared to nonobese patients10. Haverkamp et al. noted an increase in the rate of infection in obese individuals with an odds ratio of 0.3 and an occurrence of 3 times more often in obese individuals compared to patients with normal weight14.
Orthopedic surgeons have been exploring strategies to mitigate the increased infection risks observed in obese patients undergoing arthroplasty. One such approach is the administration of extended oral antibiotics as a post-operative prophylactic measure. However, accepting this practice as the standard of care remains to be determined due to inconclusive results reported in the current literature. Carender et al. recently examined the efficacy of extended oral antibiotic prophylaxis in morbidly obese patients undergoing total joint arthroplasty. Their findings did not show a significant difference in wound complications (11% vs. 8%; P = .41) or prosthetic joint infection (PJI) rates (1.7% vs. 0.6%; P = .35) between the group receiving antibiotic prophylaxis and the group without prophylaxis16.
In contrast, Inabathula et al. reported a 2.2% reduction in the risk of postoperative THA infections within 90 days among obese patients who received prophylactic oral antibiotics17. Furthermore, they found that obese patients not receiving prophylaxis had an odds ratio of 4.0 (p = 0.037) for developing PJI following THA17. While the data regarding using extended oral antibiotics prophylactically in obese patients remains controversial, Lipson et al. argue that the practice is cost-effective. Their study reported that prophylactic antibiotics post-operatively in obese patients were associated with an absolute reduction risk of 0.151%, although, in the setting of a relatively large number needed to treat (NNT = 662)18.
THA Dislocation Rate
Dislocation following THA has been consistently higher than in obese patients, regardless of surgical approach10,13,14. Onggo et al. noted obese patients had a higher rate of postoperative dislocations with an odds ratio of 1.72 (p < 0.001)13. Other meta-analyses, such as Liu et al., and Haverkamp et al., showed similar findings with a relative risk of 2.08 (p < 0.0001) and an odds ratio of 0.54, respectively, demonstrating higher rates of dislocation in obese individuals following THA as well10,14. The rate of dislocation also significantly increases incrementally in super-obese individuals when compared to patients with a BMI < 40 kg/m2 (3.3%, six-month risk, p < 0.001), as demonstrated in Werner et al.11.
Periprosthetic fracture
The correlation between periprosthetic fracture in obese patients undergoing THA is not as defined, as well as infection and dislocation rates in this population. In a retrospective cohort study, Jeschke et al. analyzed 131,576 THAs and found the risk of periprosthetic fractures was significantly higher in patients with a BMI > 40 kg/m2 (OR 1.5, 1.7% vs. 1.0 % for BMI < 30 kg/m2, p < 0.001)20. Another retrospective study performed in Japan by Iwata et al., consisting of 62 THAs (31 obese hips), showed avulsion fractures of the greater trochanter occurring three times higher in obese patients than nonobese patients. However, this value was not statistically significant (p = 0.31)21. In a retrospective cohort study including more than 14,000 THAs and more than 300 periprosthetic fractures, BMI was not associated with a periprosthetic fracture22. Given these conflicting results and relatively little data, the risk of periprosthetic fractures in obese patients following THAs requires further study.
Venous Thromboembolism
Evidence also suggests obese individuals are likelier to experience VTE12-14. A prospective study of 1231 consecutive patients treated for VTE found that 96% had at least one recognized risk factor, and 37.8% were obese23. Despite this prevalence, studies have found no association of VTE based solely on excess weight, and etiology is likely multifactorial24. Haverkamp et al. analyzed seven studies totaling 3,716 patients noting an odds ratio of 0.56 (p = 0.04) [14]. Others have noted a much higher rate of VTE following THA (5.8%) in super-obese individuals (BMI > 50 kg/m2) when compared to nonobese, obese, and morbidly obese patients (p < 0.0001 for all categories)12.
Role of preoperative bariatric surgery
Given the high rates of complications following THA in obese patients, there has been significant interest in researcher methods for reducing the risk of postoperative complications, such as bariatric surgery. However, the literature surrounding the role of preoperative weight loss via bariatric surgery prior to THA remains controversial25,26,27. In a meta-analysis review totaling 23,348 patients who underwent either THA or TKA (657 patients who had undergone bariatric surgery), there were no statistically significant differences in outcomes in superficial or deep wound infection(s), VTE, or need for revision surgery, between the two groups25. These findings suggest complication rates in obese patients are not solely due to BMI and are multifactorial. Further study indicated that analysis of postoperative complications in this meta-analysis was assessed as a ‘very low’ quality of evidence using the GRADE approach. Therefore, confidence remains low due to inconsistency, imprecision, and risk of bias25.
Other published literature surrounding bariatric surgery before THA include Parvizi et al., which looked at 20 patients with a mean BMI of 49 kg/m2 who underwent bariatric surgery followed by total hip or knee joint arthroplasty. The mean BMI decreased to 29 kg/m2 following bariatric surgery, and for the eight patients who underwent THA, their mean HHS score improved from 40 to 67.5 (p < 0.05)28. Although significant, Y H Chee et al. reported the mean increase in HHS following THA in obese individuals who did not undergo bariatric surgery was higher than reported in Parvizi et al.’s published data (see below)29. Furthermore, Parvizi reported one incidence of aseptic loosening at five years, requiring revision, which created a complication rate of 12.5% within the study.
Current literature also suggests the timing of bariatric surgery before THA may not reduce complication rates either. Inacio et al. reported on 11,032 total joint arthroplasties (TJA) (2,653 THA’s) examining the complication rates of bariatric surgery two years before TJA (Group 1), within two years of TJA (Group 2), or no bariatric surgery (Group 3). Results showed no statistical difference in 1-year complication rates between each group (Group 1, 2.9% (95% CI 0.0–6.9%); Group 2, 5.9% (95% CI 1.3%–10.4%); and Group 3, 4.1% (95% CI 3.8%–4.5%))30. However, it should be noted these studies are purely observational, and no randomized controlled trial has directly studied the role of bariatric surgery before TJA.
Long-term outcomes
Surgeons aim to improve long-term functional mobility and pain when performing THA; therefore, examining such outcomes in obese is essential. In Haverkamp's meta-analysis, post-operative Harris Hip Scores (HHS) were compared, and nonobese patients had a mean difference of 5 points higher than obese patients, a statistically significant mean difference14. Although nonobese individuals have better functional scores following THA, the overall degree of improvement from baseline HHS and quality of life scores in obese individuals is similar according to Y H Chee et al. (HHS: 52.0 vs. 48.1, p = 0.8)29 (Figure 3). Additionally, long-term survival of hip prosthesis is not adversely affected, as noted by Yeung et al., who reviewed 2,026 consecutive primary THAs showing no difference in prosthesis survival between obese and nonobese patients at 11 years (p = 0.552)31 (Figure 4).
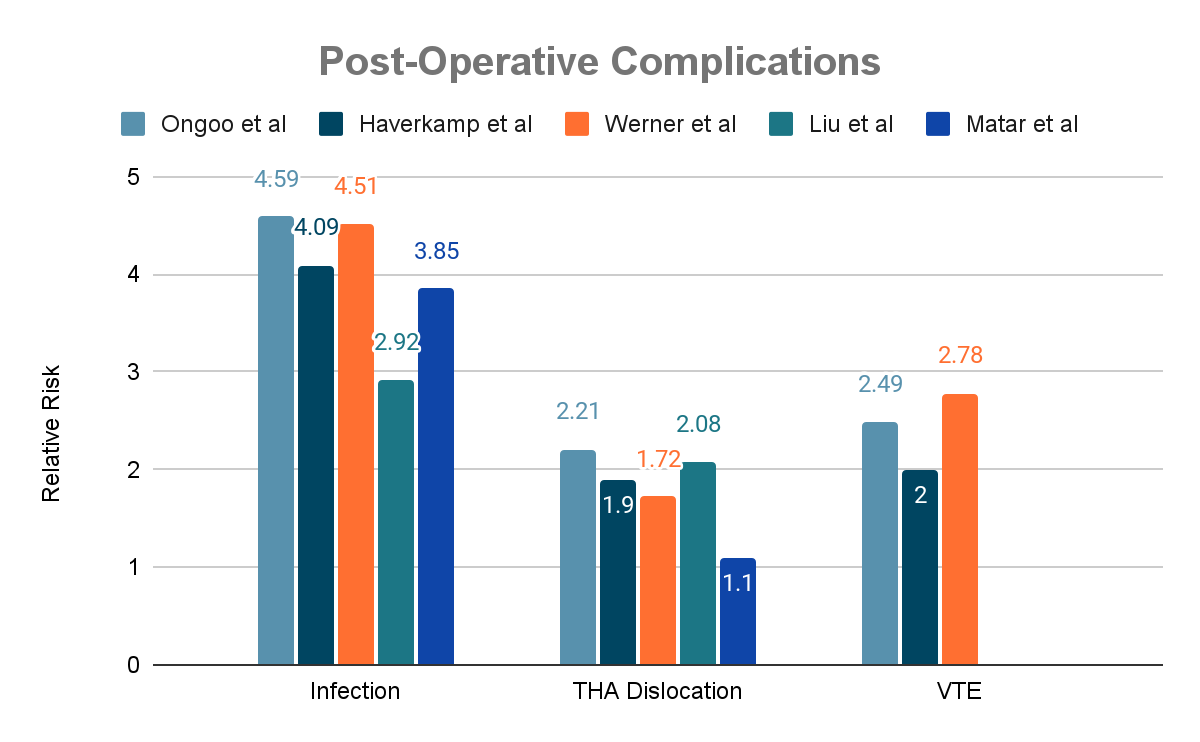
Figure 3a: Data from Ongoo et al, Haverkamp et al, Werner et al, Liu et al, and Matar et al extracted to compare relative risks between each study and the associated complications9-13
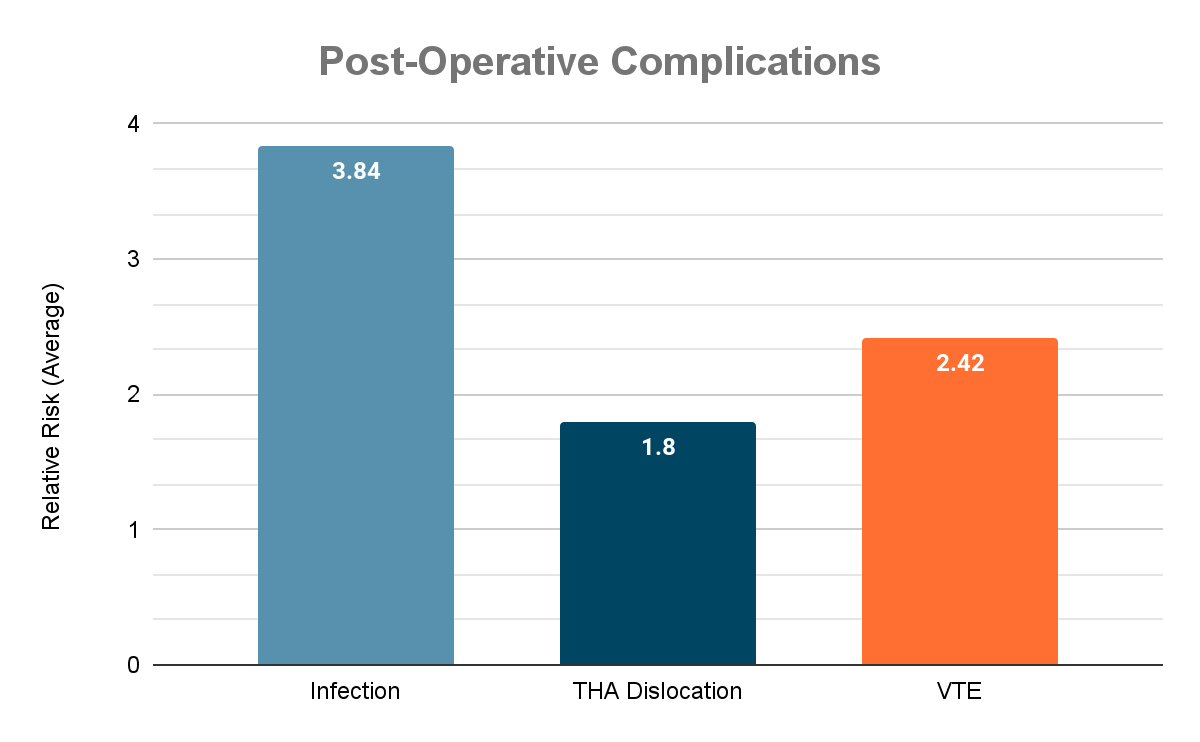
Figure 3b: Average relative risks of post-operative complications seen in Onggo et al, Haverkamp et al, Werner et al, Liu et al, and Matar et al.9-13
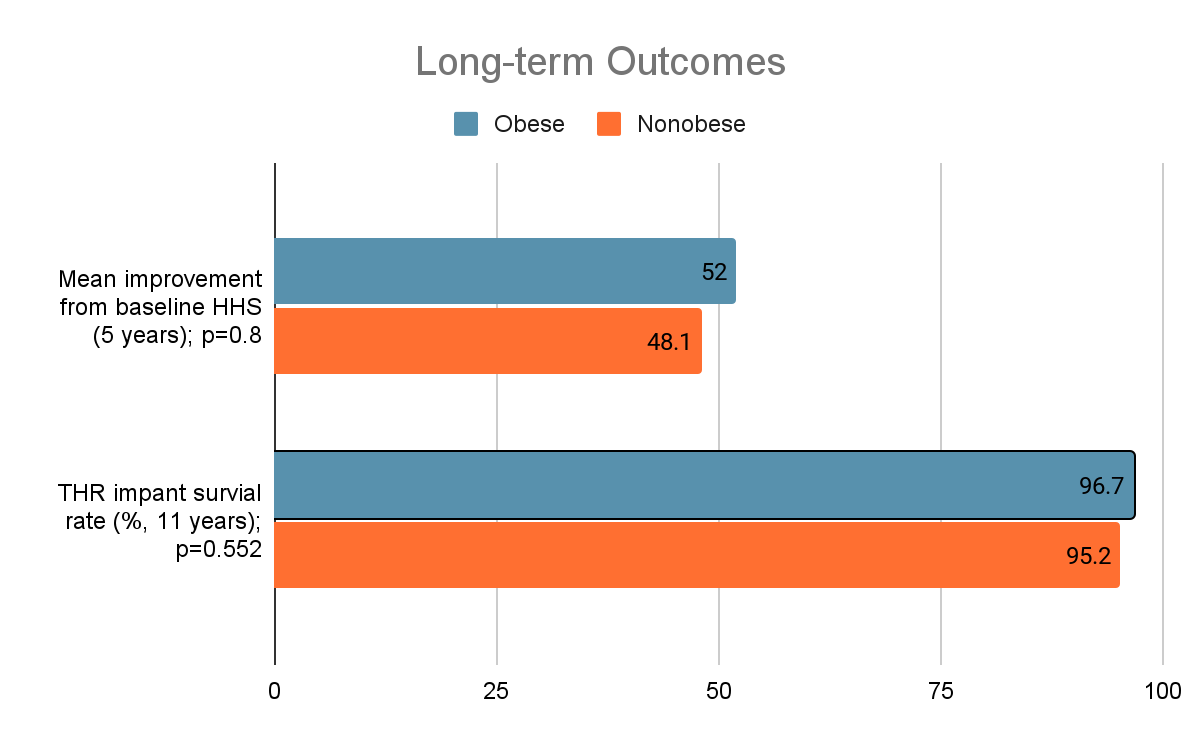
Figure 4: Long-term Outcomes examining mean HHS improvement from baseline at 5 years and THR implant survival at 11 years28,29
Discussion
This literature review sheds light on the implications of obesity on total hip arthroplasties (THA) and its associated complications. The findings consistently demonstrate that obese patients undergoing primary THA for osteoarthritis tend to do so at an earlier age compared to nonobese patients5,6. Furthermore, obesity is associated with a significantly higher risk of perioperative complications, including infections, dislocations, and venous thromboembolism10-16,23,24. Regarding infection, many theories exist on why they tend to occur more often in obese individuals. One hypothesis seen in the direct anterior approach (DAA) is a combination of immune dysfunction and proximity of the anterior incision to the inguinal crease and genitalia with overlying abdominal pannus15. Other theories suggest an increased risk of infection due to exposure difficulty, increased operation duration, denutrition, and micro-inflammation status10.
Further examining dislocation risk, Elkins et al. performed a biomechanical analysis examining the laterally directed forces during hip adduction owing to thigh-to-thigh contact and how factors under the surgeon's control (head size, neck offset, cup geometry, cup abduction) would affect stability under these conditions. The analysis attributed thigh soft tissue impingement as a mechanism that lowered resistance to dislocation for those with a BMI > 40 kg/m2, as increased thigh soft tissue impingement created an increased cup abduction angle and independently increased the risk for impingement19. Results suggested that reduced cup abduction, high neck offset, and full-cup coverage would likely reduce the risk of dislocation events, which could be considered for arthroplasty surgeons performing THA on obese patients19.
Despite the increased rate of perioperative complication risks in obese individuals undergoing primary THA, the long-term survival of prostheses is similar to nonobese patients29. Additionally, the degree of improvement in HHS scores is similar to nonobese patients, although nonobese patients tend to have higher scores pre- and post-operatively28. Given these findings, the decision to perform THA on obese patients should not be solely based on BMI, and other factors, such as management of comorbidities, surgical exposure, and nursing care, should be considered when deciding on surgical candidacy.
Providing obese patients counseling regarding their heightened risk of perioperative complications is paramount for a completely informed decision. While some arthroplasty surgeons may continue to advise preoperative weight loss before undergoing total hip arthroplasty, surgeons should acknowledge bariatric surgery before surgery in hopes of sustaining fewer complications has failed to be proven. However, data on this topic remains controversial25-30. Although controversial, all studies examining bariatric surgery concerning total joint arthroplasty have been retrospective and observational. Further studies with randomization of patients receiving preoperative bariatric surgery before THA with more standardization of study follow-up times could better answer this question.
It is also important to note using a hard cut-off based on a patient's BMI remains controversial among surgeons. While BMI is a commonly used metric to assess obesity, it does not capture the full complexity of an individual's health status. The decision to perform total hip arthroplasty (THA) should involve a thorough evaluation of various factors, including the patient's overall health, comorbidities, surgical risk, and potential benefits of the procedure. By developing more nuanced and personalized criteria for surgical candidacy, surgeons can consider individual patient characteristics outside of their BMI, which may lead to better outcomes for obese patients undergoing THA. However, this highlights the need for further research to establish evidence-based guidelines and optimize decision-making in the obese population.
Considering the limitations of this literature review, it is important to note that the correlations between obesity and THA complications are primarily derived from retrospective studies and meta-analyses that may contain overlapping datasets. While the repetition of findings does not diminish their strength, it is essential to exercise caution when interpreting these results to avoid potential misrepresentation. Additionally, the study selection process was not conducted systematically, restricting this comprehensive analysis of the current literature to a review. The first author was the only one to complete the review process and interpret study data, potentially creating a selection bias. Furthermore, multiple reviewers did not independently assess the articles, and inter-rater reliability was also not evaluated.
Despite these limitations, the existing body of literature strongly supports increased complication rates in obese patients undergoing THA. This phenomenon is not solely attributable to biomechanical forces but is multifactorial, involving inflammatory and genetic predispositions that warrant further investigation. Continued research efforts are necessary to gain a more comprehensive understanding of the underlying mechanisms and to develop evidence-based interventions to mitigate the risks associated with obesity in the context of THA. By addressing these gaps in knowledge, we can strive for improved outcomes and better patient care in this population.
Declarations
Funding
No funding was obtained to support this article.
Conflicts of Interest
The authors have no conflicts or competing interests to disclose.
Ethics Approval
Not applicable
Consent to Participate
Not applicable
Consent for Publication
Not applicable
Availability of Data and Material
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
Code Availability
Not applicable
Authors' Contributions
Ryan Bialaszewski, PA-C, contributed to the literature review article in its entirety, including conceiving the presented idea, performing a literature review, writing the manuscript, and calculating of average relative risks between studies presented in the article. Robert H. Ablove, MD, provided critical feedback and helped shape the research, analysis, and manuscript.
References
- Obesity and overweight. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Published June 9, 2021. Accessed June 12, 2022.
- Adult obesity facts. Centers for Disease Control and Prevention. https://www.cdc.gov/obesity/data/adult.html. Published May 17, 2022. Accessed June 12, 2022.
- Defining adult overweight & obesity. Centers for Disease Control and Prevention. https://www.cdc.gov/obesity/basics/adult-defining.html. Published June 3, 2022. Accessed June 12, 2022.
- Haynes J, Nam D, Barrack RL. Obesity in total hip arthroplasty: does it make a difference? The Bone & Joint Journal. 2017; 99-B(1_Supple_A): 31-36. https://doi.org/10.1302/0301-620x.99b1.bjj-2016-0346.r1
- Kumar P, Sen RK, Aggarwal S, et al. Common hip conditions requiring primary total hip arthroplasty and comparison of their post-operative functional outcomes. Journal of Clinical Orthopaedics and Trauma. 2019; 11(Suppl 2): S192-S195. https://doi.org/10.1016/j.jcot.2019.02.009
- Koonce RC, Bravman JT. Obesity and osteoarthritis: more than just wear and tear. J Am Acad Orthop Surg. 2013; 21(3): 161-169. https://doi.org/10.5435/JAAOS-21-03-161
- Abdulla I, Mahdavi S, Khong H, et al. Does body mass index affect the rate of adverse outcomes in total hip and knee arthroplasty? A retrospective review of a total joint replacement database. Canadian Journal of Surgery. 2020; 63(2): E142-E149 https://doi.org/10.1503/cjs.006719
- Andrew JG, Palan J, Kurup HV, et al. Obesity in total hip replacement. The Journal of Bone and Joint Surgery British volume. 2008; 90-B(4): 424-429. https://doi.org/10.1302/0301-620x.90b4.20522
- Lübbeke A, Stern R, Garavaglia G, et al. Differences in outcomes of obese women and men undergoing primary total hip arthroplasty. Arthritis & Rheumatism. 2007; 57(2): 327-334. https://doi.org/10.1002/art.22542
- Liu W, Wahafu T, Cheng M, et al. The influence of obesity on primary total hip arthroplasty outcomes: A meta-analysis of prospective cohort studies. Orthopaedics & Traumatology: Surgery & Research. 2015; 101(3): 289-296. https://doi.org/10.1016/j.otsr.2015.01.011
- Matar HE, Pincus D, Paterson JM, et al. Early surgical complications of total hip arthroplasty in patients with morbid obesity: Propensity-matched cohort study of 3683 patients. The Journal of Arthroplasty. 2020; 35(9): 2646-2651. https://doi.org/10.1016/j.arth.2020.04.044
- Werner BC, Higgins MD, Pehlivan HC, et al. Super Obesity is an independent risk factor for complications after primary total hip arthroplasty. The Journal of Arthroplasty. 2016; 32(2): 402-406. https://doi.org/10.1016/j.arth.2016.08.001
- Onggo JR, Onggo JD, de Steiger R, et al. Greater risks of complications, infections, and revisions in the obese versus non-obese total hip arthroplasty population of 2,190,824 patients: A meta-analysis and systematic review. Osteoarthritis and Cartilage. 2019; 28(1): 31-44. https://doi.org/10.1016/j.joca.2019.10.005
- Haverkamp D, Klinkenbijl MN, Somford MP, et al. Obesity in total hip arthroplasty—does it really matter? Acta Orthopaedica. 2011; 82(4): 417-422. https://doi.org/10.3109/17453674.2011.588859
- Purcell RL, Parks NL, Gargiulo JM, et al. Severely obese patients have a higher risk of infection after direct anterior approach total hip arthroplasty. The Journal of Arthroplasty. 2016; 31(9): 162-165. https://doi.org/10.1016/j.arth.2016.03.037
- Carender CN, DeMik DE, Glass NA, et al. Do extended oral postoperative antibiotics prevent early periprosthetic joint infection in morbidly obese patients undergoing primary total joint arthroplasty? The Journal of Arthroplasty. 2021; 36(8): 2716-2721. doi:10.1016/j.arth.2021.03.018
- Inabathula A, Dilley JE, Ziemba-Davis M, et al. Extended oral antibiotic prophylaxis in high-risk patients substantially reduces primary total hip and knee arthroplasty 90-day infection rate. Journal of Bone and Joint Surgery. 2018; 100(24): 2103-2109. doi:10.2106/jbjs.17.01485
- Lipson S, Pagani NR, Moverman MA, et al. The cost-effectiveness of extended oral antibiotic prophylaxis for infection prevention after total joint arthroplasty in high-risk patients. The Journal of Arthroplasty. 2022; 37(10): 1961-1966. doi:10.1016/j.arth.2022.04.025
- Elkins JM, Daniel M, Pedersen DR, et al. Morbid obesity may increase dislocation in total hip patients: A biomechanical analysis. Clinical Orthopaedics & Related Research. 2013; 471(3): 971-980. https://doi.org/10.1007/s11999-012-2512-3
- Jeschke E, Citak M, Günster C, et al. Obesity increases the risk of postoperative complications and revision rates following primary total hip arthroplasty: An analysis of 131,576 total hip arthroplasty cases. The Journal of Arthroplasty. 2018; 33(7): 2287-2292.e1. https://doi.org/10.1016/j.arth.2018.02.036
- Iwata H, Sakata K, Sogo E, et al. Total hip arthroplasty via an anterolateral supine approach for obese patients increases the risk of greater trochanteric fracture. Journal of Orthopaedics. 2018; 15(2): 379-383. https://doi.org/10.1016/j.jor.2018.03.005
- Singh JA, Jensen MR, Harmsen SW, et al. Are gender, comorbidity, and obesity risk factors for postoperative periprosthetic fractures after primary total hip arthroplasty? The Journal of Arthroplasty. 2013; 28(1): 126-31.e1-2. https://doi.org/10.1016/j.arth.2012.03.010
- Anderson FA, Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003; 107(23_suppl_1): I9-16. https://doi.org/10.1161/01.cir.0000078469.07362.e6
- Heit JA, Silverstein MD, Mohr DN, et al. Risk factors for deep vein thrombosis and pulmonary embolism. Archives of Internal Medicine. 2000; 160(6): 809. https://doi.org/10.1001/archinte.160.6.809
- Smith TO, Aboelmagd T, Hing CB, et al. Does bariatric surgery prior to total hip or knee arthroplasty reduce post-operative complications and improve clinical outcomes for obese patients? The Bone & Joint Journal. 2016; 98-B(9): 1160-1166. https://doi.org/10.1302/0301-620x.98b9.38024
- Gu A, Cohen JS, Malahias M-A, et al. The effect of bariatric surgery prior to lower-extremity total joint arthroplasty: A systematic review. HSS Journal®. 2019; 15(2): 190-200. https://doi.org/10.1007/s11420-019-09674-2
- Bookman JS, Schwarzkopf R, Rathod P, et al. Obesity: The Modifiable Risk Factor in Total Joint Arthroplasty. Orthopedic Clinics of North America. 2018; 49(3): 291-296. https://doi.org/10.1016/j.ocl.2018.02.002
- Parvizi J, Trousdale RT, Sarr MG. Total joint arthroplasty in patients surgically treated for morbid obesity. The Journal of Arthroplasty. 2000; 15(8): 1003-1008. doi:10.1054/arth.2000.9054
- Chee YH, Teoh KH, Sabnis BM, et al. Total hip replacement in morbidly obese patients with osteoarthritis: results of a prospectively matched study. J Bone Joint Surg Br. 2010; 92(8): 1066-1071. https://doi.org/10.1302/0301-620X.92B8.22764
- Inacio MCS, Paxton EW, Fisher D, et al. Bariatric surgery prior to total Joint Arthroplasty may not provide dramatic improvements in post-arthroplasty surgical outcomes. The Journal of Arthroplasty. 2014; 29(7): 1359-1364. doi:10.1016/j.arth.2014.02.021
- Yeung E, Jackson M, Sexton S, et al. The effect of obesity on the outcome of hip and knee arthroplasty. International Orthopaedics. 2010; 35(6): 929-934. https://doi.org/10.1007/s00264-010-1051-3
