Posterior L5 Transversectomy and Decompression for Far-out Syndrome caused by Lumbosacral Transitional Vertebra: A Case Report
Zhian Chen1,2, Hongbo Tan2, Tianhua Zhou2, Yongqing Xu2, Yi Cui2, Yang Li2, Rongmao Shi2*
1Kunming Medical University, Kunming, Yunnan, China
2Department of Orthopaedic Surgery, People's Liberation Army Joint Logistic Support Force 920th Hospital, Kunming, Yunnan, China
Abstract
Far-out syndrome is an unusual type of Bertolotti’s syndrome refers to L5 nerve root compressed by osteophyte in the extraforaminal zone, which leads to radical pain of the leg by radiculopathy. Conservative treatment is generally ineffective and requires operative decompression. We present the case of a 19-years-old patient complained of pain in the right lumbosacral and lower leg, failed for 2 months of conservative treatment. The patient was confirmed as far-out syndrome by imaging examinations showed the right L5 nerve root compressed by osteophytes from pseud arthrosis between the L5 transverse process and sacral ala. The Visual analog scale (VAS) pain score was 6 and the Oswestry disability index (ODI) was 53.33%. Then the osteophytes and pseudarthrosis were surgical removed and the L5 nerve root was decompressed through a posterior approach. The patient’s symptoms were significantly relieved after surgery immediately. The VAS score was 1 and ODI was 15.56% at 1-month postoperatively. At 1-year follow up, the VAS pain score was 1 and ODI was 11.11% and complete military trainings was resumed.
Background
Lumbosacral transitional vertebra (LSTV) is a congenital spinal dysplasia characterized as an abnormally enlarged transverse process of the last lumbar vertebra that is articulated or fused unilaterally or bilaterally with the sacrum basis or iliac crest. In the general population, the prevalence of LSTV ranges from 4.6% to 35.9%1-4. Cases of LTSV and low back pain or sciatica are referred to Bertolotti’s Syndrome, which was first described by Mario Bertolotti in 1917. LSTV does change the biomechanics of the lumbosacral portion and may be expected to result in spinal symptoms. Whether LSTV is the main cause of low back pain or sciatica remains controversial.
LSTV was classified into 4 types by Castellvi in 19845. Type I presents unilateral (Ia) or bilateral (Ib) dysplastic transverse processes, measuring at least 19mm in width. Type II exhibits incomplete unilateral (IIa) or bilateral (IIb) lumbarization/sacralization with an enlarged transverse process that has a diarthrodial joint between itself and the sacrum. Type III LSTV describes unilateral (IIIa) or bilateral (IIIb) lumbarization/sacralization with complete osseous fusion of the transverse process(es) to the sacrum. Type IV exhibits type II on one side and type III on the other. As a rare clinical case type of Bertolotti’s syndrome, far-out syndrome refers to L5 nerve root radiculopathy caused by osteophytes of the articulation between the transverse process of the transitional vertebra and the sacrum; only a few small clinical series and case reports have been published. Here, we report a case of far-out syndrome with Castellvi type IIa LSTV. The patient underwent posterior L5 decompression by transversectomy and pseudoarthrotomy and achieved satisfactory pain relief.
Case Report
A 19-year-old male soldier complained of pain in the right lumbosacral region and leg. He was given NSAID drug treatment and advised to rest. A month later, the pain was relieved, and he returned to military training. But the low back and leg pain were recurrenced and more worse, which prevented him from participating in the training normally. During daily activities, symptoms worsen when bending and coughing, and the pain worsens when walking 50 meters. It is necessary to sit down and rest. The symptoms persist for 4 days, and repeated protection and treatment are ineffective, so he was sent to our hospital and admitted to the orthopedic department. Lumbar radiography indicated LSTV and an articulation between the right L5 transverse process and the ala of the sacrum. His visual analog scale (VAS) pain score was 6 and the Oswestry disability index (ODI) was 53.33%. On clinical examination, slight hypoesthesia over the right L5 dermatome was found. The straight leg raising test of the right leg was positive at 40 degrees, and the right piriformis muscle tension test was positive. The muscle strength of the right lower limb and the deep reflex of the right lower limb were normal, and all pathological signs were negative.
The X-rays of lumbar spine demonstrated the right abnormally enlarged transverse process of L5 articulated with the sacral ala (Castellvi type IIa) [Figure 1a]. Computed Tomography (CT) 3D reconstruction showed osteophyte formation of medial pseudarthrosis [Figure 1b]. Axial computed tomography [Figure 1c] and T2-weighted magnetic resonance imaging (MRI) [Figure 1d] suggested impingement of the right L5 nerve root between the medial vertebral bone and the lateral pseudoarticular osteophyte at the far-out zone of the vertebral foramen. Coronal magnetic resonance imaging showed that the right L5 nerve root was compressed by osteophytes from medial pseudarthrosis between the L5 transverse process and sacral ala [Figure 1e]. MRI of the lumbar spine and hip demonstrated no lumbar disc herniation of L4/5 or lesions around the right piriformis muscle.

Figure 1: The white arrow indicates the osteophyte, and the black arrow indicates the right L5 nerve root. (1a) Positive position of preoperative radiograph. (1b, c) Preoperative computed tomography images. (1b) 3D reconstruction. (1c) Cross section. (1d, e) Preoperative magnetic resonance images. (1d) Cross section. (1e) Coronal section.
Firstly, a piriformis tendon block was performed using 1% lidocaine, but the leg pain was not relieved. Three days later, a transforaminal selective right L5 nerve root block was performed by using 1.5 ml 1% lidocaine with X-ray guidance, and the leg pain relieved for 12 h. This selective nerve root block (SNB) suggested that the leg pain might be originated from the right L5 nerve root. Based on the patient’s symptoms, physical examinations, imaging manifestations and SNB findings, we supposed that the right L5 nerve root impinged by the osteophyte of medial enlarged pseudarthrosis was the main cause of the leg pain, and the lumbosacral pain was mostly originated from pseudarthrosis formed by enlarged transverse process of L5 and sacral ala.
Enlarged transverse process and pseudarthrosis resection of the right L5 were performed through a posterior approach in the prone position. Briefly, an 8-cm longitudinal paramedian incision was made at the lateral border of the right erector spine muscles centered over the level L5 spinous process. The lumbar fascia was dissected, and the interval between the erector spine muscles and the multifidus were found. Dissection proceeded between these two muscles and the right transverse process of L5 was exposed and confirmed by C-arm fluoroscopy. The entire enlarged transverse process was removed using a laminar rongeur, and the proximal medial portion of the sacral ala and its osteophytes, was also carefully removed by using a high-speed drill. The L5 root was carefully separated from the surrounding tissues and identified along its course using a freer dissector. After osteotomy, we found that the L5 nerve root sheath completely expanded, and the anterior exit zone of the root foramen was adequately decompressed. Finally, C-arm fluoroscopy was used to confirm that the entire pseudarthrosis and osteophytes had been completely removed. A postoperative lumbar spine plain radiograph [Figure 2a] and CT 3D reconstruction [Figure 2b] showed the enlarged transverse process, and pseudarthrosis was completely resected.
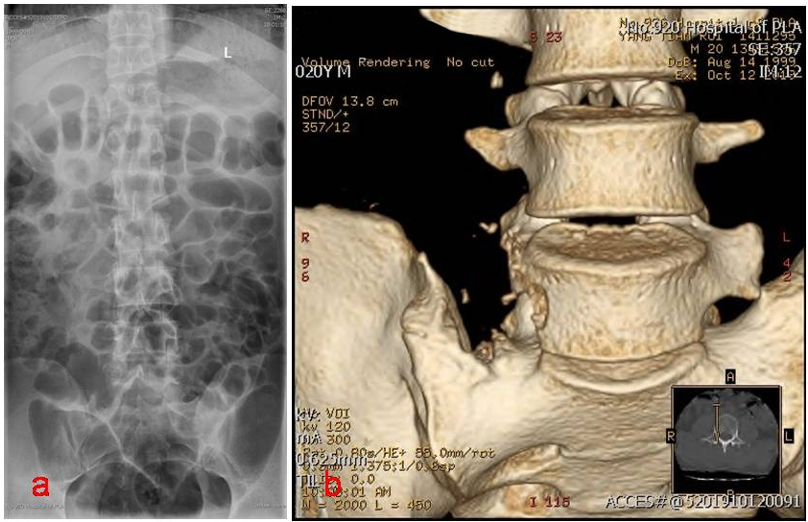
Figure 2: (2a) Positive position of postoperative radiograph. (2b) 3D reconstruction of Postoperative computed tomography images.
After surgery, lumbosacral and the leg pain was relieved immediately (VAS pain score was 2), and the straight leg raising test of the right leg was negative. One month later, VAS pain score was 1, and ODI was 15.16%, the patient begun to resume military training. At 1-year follow up, the VAS pain score was 1 and ODI was 11.11% and complete military training was resumed.
Discussion
In anatomical, the L5 nerve root could be entrapped inside the “lumbosacral tunnel” formed by the L5 vertebrae, sacral ala and the lumbosacral ligament, and very often, the L5 nerve was found to be compressed by osteophytes or by the lumbosacral ligament while passing through this tunnel. In an anatomical study, Matsumote dissected 29 geriatric cadavers, and entrapment of the L5 spinal nerve in the lumbosacral tunnel was observed in six of seven cadavers with L5–S1 osteophytes but in only one of the 22 cadavers without such osteophytes. The authors concluded that osteophytes of L5–S1 vertebral bodies were one of the causes of the entrapment of the L5 nerve and led to radiculopathy6. This compression of the nerve root by medial osteophytes is more common in older patients, which have been confirmed in clinical cases7,8. However, for LSTV patients, the intervertebral level below the transitional vertebra was described to be more stable, more protective against mechanical stress and less likely to progress degenerative change Therefore, the incidence of disc herniation, spinal stenosis, instability and osteophyte formation in this segment is decreased, which indicate that L5 nerve roots compressed by osteophytes form the vertebral body should not be common in young patients. Instead, the nerve root was compressed by lateral pseudoarticular osteophytes between the transverse process and the sacral ala is more often9,10.
Previous reports have demonstrated that coronal MRI of the lumbosacral junction and sacrum was useful in the assessment of extraforaminal stenosis and radicular symptoms11. Selective radiculography and selective nerve root block were also effective methods to identify the compressed nerve root. For this patient, CT and MRI clearly showed that the right L5 nerve root was compressed by the pseudoarticular osteophyte, but we also performed the right L5 nerve root block to verify the source of leg pain. The pain symptoms of soldiers have significantly alleviated, and intraoperative observations have confirmed the results of CT. Therefore, we believe that L5 nerve root block can be used as one of the preoperative diagnostic methods and can be compared with preoperative nerve root block and postoperative resection to observe whether the surgery is thorough.
To our knowledge, since the first case of far-out foraminal entrapment of the L5 spinal nerve below a transitional vertebra, only 15 patients with far-out syndrome have been described in previous reports.6-10, 12-15 Of these 15 patients, 8 were male and 7 were female, with an average age of 53.1 (range 29-78) years. Thirteen patients underwent selective nerve root block. Except for 4 patients reported by Matsumoto6, 5 patients were Castellvi type IIA, 5 patients were Castellvi type IIB and 1 patient were Castellvi type IIIA. Except for two conservatively treated patients, 5 patients underwent anterior approach decompression, and 7 underwent posterior approach decompression, there is no significant difference in clinical outcomes between the anterior and posterior approaches. For this case, a 19-year-old soldier was under the age of all previously reported patients. An anterior approach was easier to remove the osteophytes, whether from the medial vertebral body wall or lateral pseudarthrosis between transverse process and sacral ala, but anterior surgical access to region of the lesion was more difficult than the posterior approach. And the posterior paramedian approach was a safe, effective and easy procedures to remove the entire enlarged transverse process and osteophytes, which resulted in a good postoperative course. Arthur L Jenkins 3rd et al.16 reported Enlarged transverse process and pseudarthrosis resection, 2% of patients face surgical failure, which gradually increases over time. At the same time, case reports of patients undergoing transverse process enlargement and pseudarthrectomy show different patient outcomes. A study showed that pain improved by only 10% after 6 weeks of surgery17; Santavirta et al.18 reported that during a 9-year follow-up, 62.5% of patients observed adjacent segment disc degeneration. At the same time, we believe that the transverse process, as the starting point of the iliopsoas muscle, may lead to a decrease in iliopsoas muscle strength, but this is only a short-term complication; The reason for the occurrence of false joints may be due to instability of the lumbosacral vertebrae, so removing the false joint may cause instability to worsen and degeneration.
Lumbosacral pain and sciatica are mostly caused by lumbar intervertebral disc herniation, but very few cases may be far-out syndrome. For clinicians, when a LSTV patient with lumbosacral pain and sciatica, far-out syndrome must be enrolled in the differential diagnosis. For these far-out syndrome patients, surgical removal of pseudarthrosis and decompression nerve root through posterior approach maybe is a safe and effective method.
Author Contributions
All authors of this manuscript have contributed significantly, and all authors are in agreement with the manuscript.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
Our institution does not require Institutional Review Board approval for reporting individual cases report.
Funding
We gratefully acknowledge the funding from the Hospital Technology Program of Joint Logistic Support Force 920th Hospital (2020YGA02), and the Yunnan Province Talents Program (2018HB001). Grants from Yunnan Orthopedics and Sports Rehabilitation Clinical Medicine Research Center (202102AA310068); Yunnan Provincial Clinical Orthopaedic Trauma Medical Center (ZX20191001).
Informed Consent
Verbal informed consent was obtained from the patient for their anonymized information to be published in this article.
References
- Jancuska JM, Spivak JM, Bendo JA. A Review of Symptomatic Lumbosacral Transitional Vertebrae: Bertolotti's Syndrome. International Journal of Spine Surgery. 2015; 9: 42.
- Bron JL, van Royen BJ, Wuisman PI. The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg. 2007; 73: 687-695.
- Delport EG, Cucuzzella TR, Kim N, et al. Lumbosacral transitional vertebrae: incidence in a consecutive patient series. Pain Physician. 2006; 9: 53-56.
- Konin GP, Walz DM. Lumbosacral transitional vertebrae: classification, imaging findings, and clinical relevance. AJNR Am J Neuroradiol. 2010; 31: 1778-1786.
- Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976). 1984; 9: 493-495.
- Matsumoto M, Chiba K, Nojiri K, et al. Extraforaminal entrapment of the fifth lumbar spinal nerve by osteophytes of the lumbosacral spine: anatomic study and a report of four cases. Spine (Phila Pa 1976). 2002; 27: E169-173.
- Iwasaki M, Akiyama M, Koyanagi I, et al. Double Crush of L5 Spinal Nerve Root due to L4/5 Lateral Recess Stenosis and Bony Spur Formation of Lumbosacral Transitional Vertebra Pseudoarticulation: A Case Report and Review. NMC Case Rep J. 2017; 4: 121-125.
- Bureta CA, Yamamoto T, Ishidou Y, et al. Extraforaminal L5 Nerve Root Compression Caused by Intervertebral Osteophyte Accompanied by Lumbosacral Transitional Vertebra: A Case Treated by Anterior Approach. World Neurosurg. 2019; 127: 464-468.
- Ichihara K, Taguchi T, Hashida T, et al. The treatment of far-out foraminal stenosis below a lumbosacral transitional vertebra: a report of two cases. J Spinal Disord Tech. 2004; 17: 154-157.
- Miyoshi Y, Yasuhara T, Date I. Posterior decompression of far-out foraminal stenosis caused by a lumbosacral transitional vertebra--case report. Neurologia Medico-Chirurgica. 2011; 51: 153-156.
- Bezuidenhout AF, Lotz JW. Lumbosacral transitional vertebra and S1 radiculopathy: the value of coronal MR imaging. Neuroradiology. 2014; 56: 453-457.
- Abe E, Sato K, Shimada Y, et al. Anterior decompression of foraminal stenosis below a lumbosacral transitional vertebra. A case report. Spine (Phila Pa 1976). 1997; 22: 823-826.
- Weber J, Ernestus R-I. Transitional lumbosacral segment with unilateral transverse process anomaly (Castellvi type 2A) resulting in extraforaminal impingement of the spinal nerve. Neurosurgical Review. 2011; 34: 143-150.
- Kikuchi K, Abe E, Miyakoshi N, et al. Anterior decompression for far-out syndrome below a transitional vertebra: a report of two cases. Spine J. 2013; 13: e21-25.
- Kapetanakis S, Chaniotakis C, Paraskevopoulos C, et al. An Unusual Case Report of Bertolotti’s Syndrome: Extraforaminal Stenosis and L5 Unilateral Root Compression (Castellvi Type III an LSTV). Journal of Orthopaedic Case Reports. 2017; 7: 4.
- Jenkins AL 3rd, Chung RJ, O'Donnell J, et al. Redefining the Treatment of Lumbosacral Transitional Vertebrae for Bertolotti Syndrome: Long-Term Outcomes Utilizing the Jenkins Classification to Determine Treatment. World Neurosurg. 2023; 175: e21-e29.
- Ugokwe KT, Chen TL, Klineberg E, et al. Minimally invasive surgical treatment of Bertolotti's Syndrome: case report. Neurosurgery. 2008.
- Santavirta S, Tallroth K, Ylinen P, et al. Surgical treatment of Bertolotti's syndrome. Follow-up of 16 patients. Arch Orthop Trauma Surg. 1993; 112(2): 82-7.
