Perceptions on Sexual Activity after Total Knee and Total Hip Arthroplasty: A Mixed Method Study of Patients, Partners, and Surgeons
Rita Th. Harmsen1*, Marjolein E.M. den Ouden2, Pieter F. Schillemans3, Henk W. Elzevier1, Rob G. Nelissen1, Brenda L. Den Oudsten4
1Departments of Orthopaedics, Biomedical Data Sciences and Department of Urology and Medical Decision Making (H.W.E.), Leiden University Medical Center, The Netherlands
2Research Group Technology, Health & Care, Academy of Social Work, University of Applied Science Saxion, Enschede, The Netherlands
3Private Center of Ultra Sonography Care, NV Hoorn, The Netherlands
4Center of Research on Psychological and Somatic Disorders (CoRPS), Department of Medical and Clinical Psychology, Tilburg University, Tilburg, The Netherlands
Abstract
Background: In-depth insight into couples’ experiences of sexual activity before and after total hip arthroplasty (THA) and total knee arthroplasty (TKA) is lacking. The aim of this study was to explore patients’ and partners’ experiences, complemented by surgeons’ opinions on safe resumption of sexual activity after surgery.
Methods: Mixed method study: 1) Semi-structured interviews among sexually active couples, 1.5 years postoperatively and 2) A survey among surgeons about recommendations of sexual activity after THA/TKA.
Results: Of the 150 invited couples, 90 (60%) responded (THA: n=39; TKA: n=42). Five couples participated (THA: n=3; TKA: n=2), while 85 (94%) couples refused participation. Two themes emerged: “Couples physically and mentally adjusted to the new situation” and “Couples undoubtedly trusted the surgeon as the provider of information.” In total, 27% (47/175) of THA surgeons participated. Fifty percent agreed with the recommended sexual positions researched by Charbonnier et al. Opinions differed widely regarding when to safely resume sexual activity. Of the TKA surgeons, 36% (76/211) responded. Almost all surgeons (95%) agreed that there were no restrictions. However, some discomfort was expected when patients bend the knee or kneel during sex. Half of the surgeons indicated that providing information about sex was necessary.
Conclusions: All couples physically and mentally adapted to the new situation without considering safety measures. Patients trusted surgeons in providing safety information. Surgeons should inform patients succinct and explicitly, especially since surgeons’ recommendations showed great variability. More motion research on hip and knee may add to uniform guidelines.
Background
Every year, millions of patients worldwide undergo total hip arthroplasty (THA) or total knee arthroplasty (TKA) for symptomatic osteoarthritis (OA)1,2. Due to the improvement in the survival times of prostheses and surgical techniques, patients are operated on at both, younger and older ages3-5. Maintaining sexual activity is associated with better quality of life and well-being6-15. Although, for many patients, sexual activity is an important aspect of their lives16,17, there is still a general taboo among patients and professionals to address this issue during consultations9,18-23.
OA of the hip causes sexual difficulties, such as lower sexual frequency or functional limitations during sexual activity, caused by stiffness and pain during external rotation or abduction of the legs13-15. Sexual difficulties have been scarcely addressed in literature, particularly for the knee joint, not for the hip12-14,24-29. In addition, the quality of most studies is low to moderate24. Most hip studies have a retrospective design13,14,25 and describe that OA can affect the sexual relationships with partners15,27. Two studies even mentioned that in 20 to 30% of THA patients, sexual dysfunction was a reason to undergo surgery13,14. Other studies showed that patients may experience fear of damaging the prosthesis after surgery, which can limit sexual activity as well11,12,26. After surgery, THA is associated with improvement of sexual activity14,25,26, although the magnitude of effects varies highly24.
OA of the knee causes sexual difficulties as well and until now, this is scarcely studied. Recently, two retrospective studies report about sexual activity of patients undergoing TKA12,30. Nunley et al. found that 98% of their sexually active cohort of (THA and) TKA patients under 60 years returned to sexual activity after surgery12. In this first quantitative study, qualitative information was not incorporated. Compared to Nunley, Kazarian et al. included patients who were slightly older. They found that 60% of patients were more easily engaged in sexual activity, although only a proportion of patients showed improvement. Postoperatively 25% had less sex and 70% did not feel greater mobility or range of motion. In 54% of patients, kneeling difficulties during sex because of diminished flexion was reported30, an improvement compared to preoperatively, where almost all patients (97%) avoided to kneel during sex and needed to change their sexual positions to accommodate the knee30. Therefore, it is expected that kneeling limitations during sexual activity will need more attention in the patient information.
Previously, we conducted studies on patients’ expectations of sexual activity after THA31 and TKA32. In both studies, expectations of postoperative sexual activity were not met in up to 40% of the patients. The causes and consequences of these unmet expectations are unknown. It may be related to the above-described functional difficulties and consequences for the kneeling function during sexual activity or may be related to the lack of knowledge about what to expect, when, and how to comfortably resume sexual intercourse11,30. Wall et al. were the first to prospectively investigate the need for information. Preoperatively, 55% of the patients would like to have information about sexual activity after surgery, while postoperatively, 83% stated they were underinformed by the surgeon26. However, preoperatively patients were not aware of relevant questions. So far, difficulties during sexual activity after THA and TKA have rarely been recognized by orthopedic surgeons; consequently, the necessary patient information is not always provided14,26,33,34. More specifically, if certain sexual positions are at risk for adverse outcomes (e.g., dislocation of the hip and insert luxation of the knee), it is not clear what surgeons will advise33,35.
To date, exploration of sexual activity in patients undergoing THA and TKA has never been researched in depth and using a qualitative study. Hence, research in the context of the couples’ experiences during pre- and postoperative sexual activity is also lacking. Therefore, the aim of this study was to explore patients’ and partners’ experiences, complemented by THA/TKA surgeons’ recommendations on safe resumption of sexual activity after surgery.
Method
Study Design
A mixed method study was conducted, consisting of
1) Semi-structured interviews about pre- and postoperative perspectives of THA/TKA patients and their partners, 1.5 years after surgery.
2) A survey was conducted among THA and TKA orthopedic surgeons to gather the surgeons’ perspectives on postoperative resuming of sexual activity.
Study Population
Patients and their partners
THA and TKA patients and partners who participated in the Longitudinal Leiden Orthopedics Outcomes of Osteo-Arthritis (LOAS) Study36 and were treated in three participating hospitals (university, top referent teaching, basic/general) were invited to participate in this study.
To determine patient eligibility, medical records were screened by the orthopedic surgeon of the outpatient clinics. Patients were eligible if they had primary hip or knee OA, undergone (uni- or bilateral) THA or TKA, and had no revisions. Patients were cohabitating, living apart, or married, and were sexually active (again) or had the intention to resume sexual activity postoperatively. We excluded sexual inactive couples, patients who had stopped being sexually active before the onset of OA, and without the intention to resume sexual activity. Since it was not known who was sexually active, all 150 eligible patients received an invitation by mail:
(1) an invitation letter signed by the attending surgeon in which the patient and partner were informed about the aims and inclusion criteria, ending with the question whether they were willing (were able) to participate in an interview. Although the subject of sexuality covers a broad multidimensional area37, we informed the couples that the interview would focus on the functional aspects (sexual intercourse with a prosthesis) and that the interviews would be conducted by an orthopedic surgeon and a researcher.
(2) Two informed consent forms for both the patient and partner were provided if they decided to participate.
(3) A non-participation return form on which patients and partners could indicate why they were unwilling to participate.
(4) Return envelope with postage.
After 4 weeks, one reminder was sent. Interviews were planned by telephone and took place within 10 weeks of informed consent was obtained.
The Regional Institutional Review Board of the University Medical Centre Leiden (Zuid Holland) approved the study (Number N20.078) and determined that, according to the Dutch legislation, this study does not meet the scope of the Medical Research Involving Human Subjects Act. Patients were informed about the study protocol according to the declaration of Helsinki. Written informed consent forms were obtained from the patients and their partners prior to the start of the interviews, including consent to record the interviews.
Orthopedic surgeons
Only orthopedic surgeons who were member of the Dutch Hip Society (DHS) and Dutch Knee Society (DKS) in the Netherlands (i.e., these orthopedic surgeons can be member of both Societies). Both, the DHS and DKS are working groups of the Netherlands Orthopedic Society (NOV). As such, these orthopedic surgeons have extensive experience in THA and/or TKA surgery. They were invited to participate by post.
The addresses for the THA and TKA working groups of orthopedic surgeons were retrieved from the NOV by member lists (THA, n=147; TKA, n=211). Members living abroad and non-orthopedic surgeons were excluded. The board obtained informed consent from their members. One reminder was sent to surgeons in the TKA group. It was not possible to remind the THA surgeons of the THA working group, because we did not obtain permission of the board.
Data Collection
Interviews with patients and their partners
Patient characteristics, that is, age, duration of OA, date of surgery, operation technique for hip, duration of relationship, use of medication, comorbidities, sexual activity status, satisfaction rates were assessed using a survey. The survey also contained three self-reported VAS scores at the start of the interview: the EQ-5D health status score (VAS 0-100), a score indicating the patient’s satisfaction with the result of surgery (VAS 0-10), and a score indicating the patient’s satisfaction explicitly based on regaining sexual activity with a prosthesis (VAS 0-10).
An Interview guide (Additional File) was constructed based on prior studies of the research group and the literature24,31,32,34. This interview guide contained the following themes: significance of preoperative difficulties of sexual activity, postoperative change(s) in sexual activity, awareness of sexual expectations, and need for information about how and when to return to sexual activity safely. The topics in the interview guide were piloted in two interviews: one female hip patient and her spouse, and one female knee patient without her partner (due to his last-minute withdrawal). Based on the outcomes of the pilots, we decided to use these “Dahm-drawings” as a tool in the final interviews33 (Figure 1).
Survey among surgeons
The surgeons’ survey focused on expert opinions on THA and TKA practices and based on recommendations for regaining sexual activity after surgery. The DHS working group of the NOV was invited to comment. The survey consisted of four topics:
- The advice per sexual position (for both men and women), based on the study of Charbonnier et al. in which a virtual total hip collision simulation was performed, extrapolated from in vivo MRI positions35. This chart (Figure 1) was sent out with the advised positions for THA patients.
- The estimated risk for luxation of the prosthesis (VAS 0-10).
- The postoperative waiting time before resuming sexual activity safely. The answer options were adapted from the studies of Dahm and Wall et al.26,33.
- The surgeons’ surgical approach.
For TKA patients, the TKA workgroup survey consisted of 3 topics:
- Whether the surgeons agreed with the statement that there are no limitations for TKA patients with regard to the twelve sexual positions adapted from the study of Dahm et al.
- This chart (Figure 1) was sent out without the advised positions for THA patients.
- Whether this topic should be included in TKA patient’' information.
- The postoperative waiting time before resuming sexual activity safely. Answer options were adapted from the studies of Dahm and Wall et al.26,33.
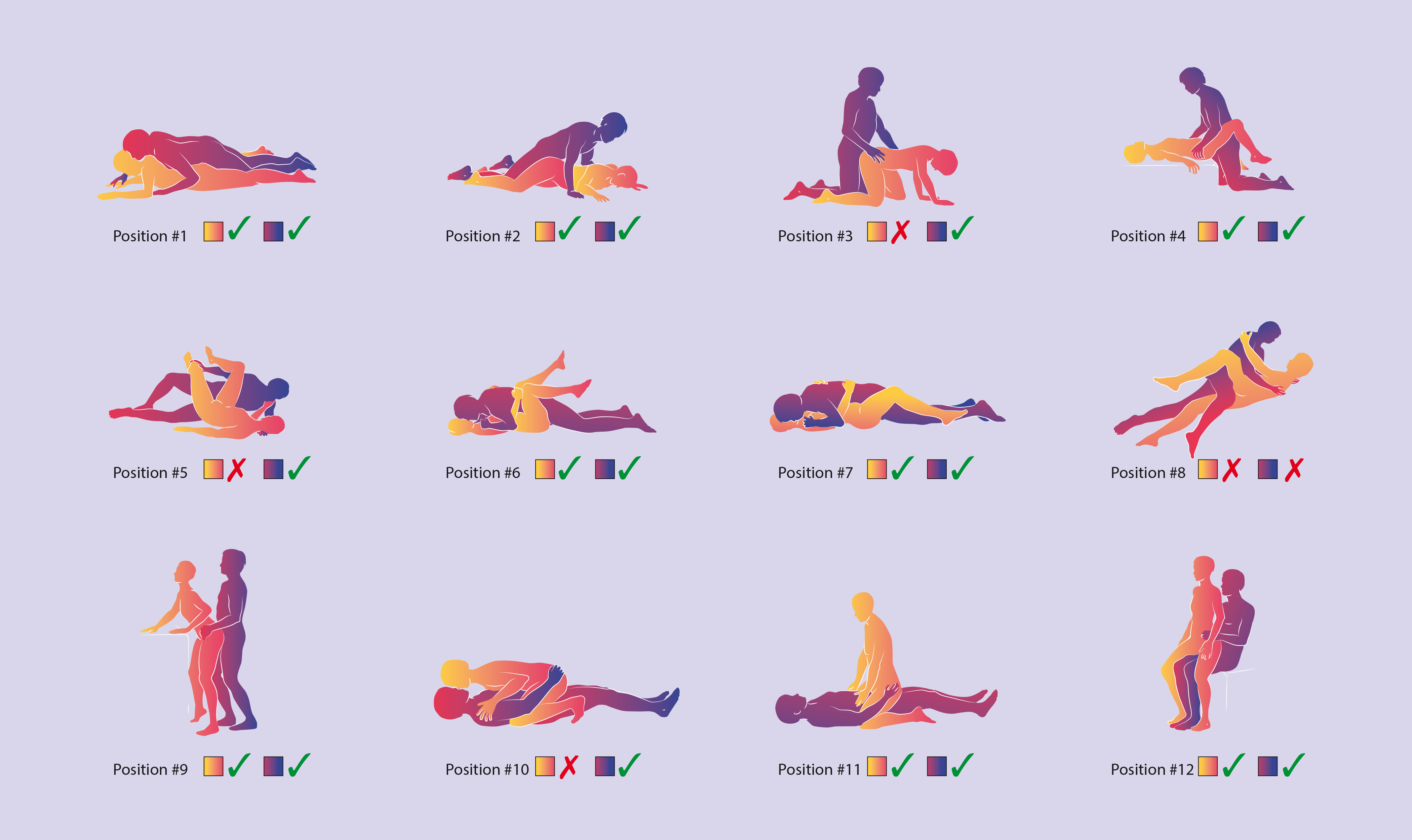
Figure 1: Twelve common sexual positions
Notes:
1 Green tick shows a “permitted” sexual position, while a red cross means that this sexual position is not advised for patients with THA by Charbonnier et al.35
2 This chart was used during the interviews with couples and for both surgeon’s survey.
For THA surgeons, the chart was sent out with recommended positions.
For TKA surgeons, the chart was sent out without recommended positions.
The chart was presented to patients and partners during the interviews without recommended positions.
The twelve sexual positions were modified from the study of Dahm and Charbonnier et al.33,35
Data Analysis
Semi-structured interviews were conducted in June 2021 at an outpatient clinic. Two researchers, RTEH (investigator) and PFS (orthopedic surgeon), conducted the interviews. PFS interviewed the couples/patients, and RTEH supervised the interviews and made field notes. All interviews were audiotaped and transcribed verbatim using Microsoft Word for Mac (version 16.66.1, 2022, Redmond, USA). For analyzing the data and to complete our work, we used the Computer Assisted Qualitative Analysis Software Program Atlas.Ti (version 9.0 Windows, Berlin, Germany).
The analyses consisted of three phases. First, transcripts were read and reread to get a first impression of “the total context” of the interviews. Second, RTEH and MDO used an iterative and inductive coding approach, following an open axial and selective coding procedure38. The interviews were coded independently, with constant discussions on interpretations and building the final code list to reach a consensus. Third, both researchers formulated themes emerging from group codes by applying the diagram affinity method39, resulting in the final themes for presentation.
Data analysis of the surveys consisted of descriptive statistics reported as frequencies and percentages for categorical data). The data were analyzed using IBM SPSS Statistics (version 24, Armonk, New York, United States).
Results
Of the 150 invited couples, 90 response forms were returned (response 60%). Five patients in a relationship were willing to participate in the interview study. These couples were eligible because they resumed sexual activity postoperatively. Eighty-five non-participation forms were received, of which 4 were incomplete, resulting in 81 non-participation forms. Of this group, 47% (n=38) were sexually inactive due to various reasons (Table 1A). The remaining group (n = 43; 53%), was sexually active and resumed without difficulties.
Eleven couples responded other reasons for non-participation, such as no time. Respondents could fill out more than one reason why they were not willing to participate. More specifically, the most common mentioned reason was that 48/81 (59%) patients felt reluctance to discuss sexual activity. About half of the THA patients (19 out of 39) and 69% (29 out of 42) of TKA patients indicated this reluctance. More females (65%) than males (53%) were reluctant. More detailed information per arthroplasty type, gender, and age groups are shown in the supplementary file Table 1B.
Table 1A: Reasons for non-participation
|
Total number of persons who declined participation# |
n = 81 (100%) |
|
Reasons for non-participation## |
140 |
|
Not Sexually Active |
38/81 (47%) |
|
Sex is no longer part of life |
13 |
|
Partner passed away |
5 |
|
Comorbidities play a role |
|
|
Patient |
14 |
|
Partner |
6 |
|
Resumed sexual activity again |
43/81 (53%) |
|
Resumed without difficulties |
38 |
|
Resumed despite age is okay |
2 |
|
Resumed despite comorbidities is okay |
3 |
|
Reluctance to discuss sexual activity |
48/81 (59%) |
|
Do not want to talk about sexuality |
19 |
|
Issue not important |
7 |
|
Too personal topic |
12 |
|
Not appropriate in conversation with an orthopedic surgeon |
5 |
|
I feel uncomfortable or ashamed to talk about sex |
5 |
|
Other reasons for non-participation |
11/81 (14%) |
|
Rehabilitation difficulties |
4 |
|
No time to participate |
3 |
|
Other |
4 |
|
# N=81/85 non-participation forms (4 forms were missing) ## More than one answer was allowed to be given (total 140 reasons). |
|
Table 1B: Reasons for non-participation per arthroplasty type, gender, age groups (Supplementary file)
|
Respondents: n=81 # |
|
Arthroplasty |
Gender |
Age groups |
|||||
|
Total |
THA |
TKA |
Men |
Women |
<65y |
65-70y |
71-75y |
>75y |
|
|
Total Respondents |
81 |
(n=39) |
(n=42) |
(n=38) |
(n=43) |
(n=25) |
(n=20) |
(n=20) |
(n=16) |
|
Total of Reasons |
140 |
(n=66) |
(n=74) |
(n=64) |
(n=64) |
(n=48) |
(n=28) |
(n=34) |
(n=30) |
|
Not Sexually Active |
38 |
24 |
14 |
19 |
19 |
4 |
12 |
12 |
10 |
|
Sex is no longer part of life |
13 |
8 |
5 |
6 |
7 |
0 |
3 |
5 |
5 |
|
Partner passed away |
5 |
4 |
1 |
1 |
4 |
1 |
3 |
0 |
1 |
|
Comorbidities play a role: |
|
|
|
|
|
|
|
|
|
|
patient |
14 |
6 |
8 |
10 |
4 |
2 |
5 |
3 |
4 |
|
partner |
6 |
6 |
0 |
2 |
4 |
1 |
1 |
4 |
0 |
|
Resuming sexual activity |
43 |
20 |
23 |
20 |
23 |
18 |
7 |
10 |
8 |
|
Resuming sexual activity (without difficulties) |
38 |
17 |
21 |
18 |
20 |
15 |
7 |
9 |
7 |
|
Resuming despite age |
2 |
1 |
1 |
1 |
1 |
0 |
0 |
1 |
1 |
|
Resuming despite comorbidities |
3 |
2 |
1 |
1 |
2 |
3 |
0 |
0 |
0 |
|
Reluctance to discuss sexual activity |
48 |
19 |
29 |
20 |
28 |
23 |
7 |
9 |
9 |
|
Do not want to talk about sexuality |
19 |
10 |
9 |
8 |
11 |
11 |
2 |
3 |
3 |
|
Sexuality as an issue is not important |
7 |
2 |
5 |
2 |
5 |
3 |
1 |
1 |
2 |
|
Too personal topic |
12 |
5 |
7 |
6 |
6 |
6 |
1 |
3 |
2 |
|
Not appropriate in conversation with a surgeon |
5 |
1 |
4 |
2 |
3 |
1 |
1 |
1 |
2 |
|
I feel uncomfortable/ashamed to talk about sexuality |
5 |
1 |
4 |
2 |
3 |
2 |
2 |
1 |
0 |
|
Other reasons for non-participation |
11 |
3 |
8 |
5 |
6 |
3 |
2 |
3 |
3 |
|
Rehabilitation difficulties |
4 |
1 |
3 |
2 |
2 |
1 |
1 |
1 |
1 |
|
No time to participate |
3 |
1 |
2 |
1 |
2 |
2 |
0 |
1 |
0 |
|
Other |
4 |
1 |
3 |
2 |
2 |
0 |
1 |
1 |
2 |
|
# N=81/85 non-participation forms (4 forms were missing). More than one answer was allowed to be given (in total 140 reasons). |
|||||||||
Perceptions on sexual activity of patients and partners
Due to the last-minute withdrawal of one partner, one male patient came alone at the time of the interview. The preoperative duration of OA ranged from 3 months (patient 4, THA, male) to 12 years (patient 5, TKA, female). All patients and partners reported health issues, except for one 65-year-old female partner (Table 2). Non-musculoskeletal diseases, such as hypertension and cardiovascular issues were the most mentioned issues. None of the patients or partners had undergone other orthopedic surgery (e.g., spine fusion). At the time of the interview none of the patients suffered of (technical) complications, except for one patient who experienced incidental pain. Except for this patient, all EQ-5D VAS scores were 80 or higher, indicating a good health status at the time of interviewing. In addition, the satisfaction scores were > 8, except for the patient with incidental pain. All patients were satisfied about regaining sexual activity with a prosthesis (Table 2).
The mean duration of the interviews was 43 minutes (range 32-55 minutes).
Table 2: Characteristics of the participants
|
Participants* |
Single 1** |
Duo - 2 |
Duo - 3 |
Duo - 4*** |
Duo – 5**** |
|
Gender patient |
Male |
Female |
Male |
Male |
Female |
|
Joint replacement* Patient Surgical Approach |
TKA (first) |
bilateral THA anterior (first) |
THA (first) posterior |
THA (second one) posterior |
TKA (first) |
|
Joint replacement (partner) |
No |
No |
No |
Bilateral THA and TKA) |
No |
|
Other orthopedic surgeries in couples (e.g., spine fusion) |
No |
No |
No |
No |
No |
|
Self-reported health issues of patient |
Lower back pain |
Hypertension Cardiovascular issues |
Hypertension Prostate and kidney issues |
Hypertension Cardiovascular problems Prostate and bladder issues |
ACNES disease |
|
Self-reported health issues of partner |
Hypertension Mental problems Osteoarthritis Migraine |
Hypertension Cancer |
Hypertension Chronic lung disease |
None |
Hypertension Mental problems Cardiovascular problems Chronic lung disease Lower back pain |
|
Age patient |
68 |
56 |
55 |
73 |
61 |
|
Age partner |
73 |
61 |
55 |
65 |
65 |
|
Duration of the relationship (in years) |
40 |
31 |
16 |
49 |
10 |
|
Time after surgery (in months) |
16 |
17 |
16 |
17 |
14 |
|
Postoperative estimated resuming time of sexual activity |
>8 weeks |
>3-4 weeks |
>8 weeks |
> 6-8 weeks |
>12 weeks |
|
EQ-5D Score VAS (0-100) # |
85 |
87 |
80 |
37## |
80 |
|
Satisfaction score related to sexual activity after surgery VAS (0-10) # |
10 |
10 |
10 |
9 |
9 |
|
Satisfaction score related to THA/TKA outcome VAS (0-10) # |
8.5 |
10 |
8 |
6 ## |
9 |
|
Abbreviations: TKA total knee arthroplasty; THA total hip arthroplasty; VAS visual analogue scale; EQ-5D Euro Quality 5 Dimensions; ACNES Syndrome Anterior Cutaneous Nerve Entrapment Syndrome VAS 100 or 10: highest score * All heterosexual couples, surgical revisions were excluded ** Single interview; partner withdraw (last minute) *** Female partner recently underwent TKA (3 months postoperatively) and reported some rehabilitation difficulties. **** Patient was occasionally dependent on a wheelchair due to fatigue. # At the time of the interview # # Pain was the most important reason for this lower score. |
|||||
Two themes emerged from the interviews
- Couples adjusted naturally the new situation: physically (to sexual positions) and mentally (to the moment they felt ready).
- Couples undoubtedly trusted the orthopedic surgeon as provider of information about safely resuming sexual activity.
Theme 1: Couples adjusted naturally the new situation: physically (to sexual positions) and mentally (to the moment they felt ready)
Preoperatively, arthritic joints physically hindered all patients. Although OA limited all couples in their daily activities, they remained sexually active. Patients indicated that they adapted to the situation. They changed their routine leg position to be comfortable and some lowered their frequency of sexual activity.
“Well, I noticed that.. uhh..with me it happens naturally.., that you also adjust in your being together... unnoticed…, with the fact that with certain positions, you do act more cautiously by saying, watch out..., or.. be carefully…..but of course it happens gradually” (female patient 2, bilateral THA).
The presence of preoperative pain was predominantly mentioned as a factor contributing to the loss of quality of life. Patients were hindered during activities of daily living, sports, and recreational activities.
“Yes, it was from being able to walk for a full day to only being able to walk for an hour... well, and since we really like walking that was a thing.... , but I didn't perceive a lot of pain during sex” (male patient 3, THA).
This couple (no. 3) had the routine of being sexually active every weekend. They worked a lot during the week and found sexual activity important. They noted that despite OA, it was nice to experience that sex still was possible without pain. The couple enjoyed being sexually active and it was pleasurable for both. It brought a mind-set and focus on intimacy instead of impairment, especially since their favorite long-distance walking was no longer possible. Postoperatively, couples adjusted in a natural way as well. They all resumed sexual intercourse after surgery the moment they felt ready again. Four couples reported that this moment was approximately at the time of the check-up photo appointment at the outpatient clinic (6 to 8 weeks after surgery).
“I was very deliberately… took the warnings seriously and waited until the 6 weeks were over and the check-up X-ray was taken.... (male patient 3, THA). “His wife continued: "I don't remember thinking about safe resumption; I was really only concerned with …well…, he's having surgery, he has to recover for 6 weeks.. and we have to arrange things…, how is he going to exercise again, with those crutches, and... eh.. that walker ... (spouse patient 3)".
“The first month you are really rehabilitating, then you don't have a desire for sex. When you feel you like to do it again... then you just do it”.. (female patient 2, bilateral THA).
Safe handling of the prosthesis during sexual activity was hardly an issue. None of the participants had seriously considered potential risks. The fear of damaging the prosthesis did not play a role in waiting to resume sexual activity.
“We had no fear of damage; however, we have quite a limitation with all our prostheses”, the wife said looking to the drawings of the positions… (spouse patient 4).
Only one partner had experienced fear of hurting his wife (patient with bilateral THA) and was afraid to inflict pain. However, as his wife was not scared at all, he had not brought up his concern to her. His wife quoted: “Of course it was a thing, but I felt that it was nice again. And I think when you're together for a long time you look for ways that are pleasant”.
All respondents (retrospectively) assumed that sexual activity would not get worse after surgery and might even improve compared to preoperative experiences. For TKA, none of the patients mentioned inconveniences. The female TKA patient (no. 5) was satisfied that she had been treated after 12 years of waiting for surgery. The private circumstances of the male patient (no.1) temporarily reduced this couple’ sexual activity. In addition, during his interview, he pointed out that his preferred sexual position did not require him to bend the knees.
Theme 2: Couples undoubtedly trusted the orthopedic surgeon as provider of information about safely resuming sexual activity
Patients scheduled for surgery received general information in a booklet. Patients considered this information to be complete, assuming that all relevant topics were included. “The information is actually very good; everything is done very carefully and to the point. You also get a whole booklet yes, everything according to protocol…, so why not add something about sex, for sure this could be added…? (spouse patient 2).
None of the respondents remembered that the topic of sexual activity was mentioned by the surgeon postoperatively. All implicitly expected that orthopedic surgeons would bring up relevant issues, including advice on sexual activity, when this would be important.
“I thought it will be alright; I had confidence in him... And I also experienced something like … uh…. the orthopedic surgeon will of course warn me for something, isn’t?” (female patient 2, bilateral THA). Almost all patients and partners retrospectively stated that they had no questions about sexual activity during the consultation, except for one couple. This couple was reluctant to ask questions about safe resumption during the orthopedic consultation and tried to find answers on the internet. All participants stated that they would have wanted to know if there was a chance of damaging the prosthesis during the resumption of intercourse. They all trusted that the surgeon would inform them about important topics.
Perceptions on sexual activity of surgeons
Approximately 27% (n=47/175) of THA orthopedic surgeons completed the questionnaire. Of this group, 38.3% (n=18) performed the anterior approach, 44.7% (n=21) performed the posterior approach, 6% (12.8%) performed both approaches, and 4.3% (n=2) performed the direct-lateral approach. In addition, we asked surgeons about which positions were permitted based on the results of Charbonnier and colleagues35 (Figure 1). In total, 25 (53.2%) answered that Charbonnier’s advice could be used as a guideline for THA patients, while 20% of the surgeons (n=9) indicated that this advice could not be used. Thirteen THA surgeons (28%) answered that every sexual position was safe. The estimated risk of luxation was rated as low (VAS score: 3 or lower).
We asked the surgeons for their opinions regarding the waiting time to resume sexual activity. Regardless of the surgical approach, opinions differed. About 30 to 40% of the surgeons felt that sexual activity could be immediately resumed as soon as the patient feels ready, while others (30-40%) advised a waiting period with a duration of 6 to 8 weeks (Table 3).
Table 3: Perspectives of THA surgeons: waiting time per approach
|
Waiting time for resuming sexual activity after surgery** |
Total |
Anterior approach |
Posterior approach |
Posterior and Anterior approach* |
Direct-lateral approach |
|
N |
47 |
18 |
21 |
6 |
2 |
|
Immediately, as soon as the patient feels ready |
17 (36.2%) |
7 (38.9%) |
7 (33.3%) |
3 (50%) |
0 |
|
after 2 to 4 weeks |
3 (6.4%) |
3 (16.7%) |
0 |
||
|
after 6 to -8 weeks |
20 (42.6%) |
6 (33.3%) |
9 (42.9%) |
3 (50%) |
2 (100%) |
|
after 3 months |
4 (8.5%) |
2 (11.1%) |
2 (27.8%) |
0 |
|
|
Missing |
3 (6.4%) |
3 (16.7%) |
0 |
||
|
* These surgeons used both approaches; advice per approach is not given. ** Scales were adapted from the study of Dahm et al., and Wall et al. (26,33) |
|||||
Approximately 36% (n=76/211) of TKA surgeons returned the survey and 95% agreed that there were no restrictions on postoperative sexual activity based on the sexual positions (Figure 1). These surgeons agreed that sexual activity was immediately allowed as soon as patients felt ready. The remaining surgeons (5%) did not agree. They stated that there was a risk of dislocation of the insert, especially regarding sexual positions that required deep flexion of the knee. Fifty percent of surgeons agreed that deep bending might cause inconvenience, for instance, for men and women who used position 3 and for women who used positions 10 and 11 (Figure 1). Approximately half (51.3%) of the surgeons indicated that providing information about sexuality to patients after surgery was necessary, while the other half (47.3%) did not agree.
Discussion
This mixed method study explored THA/TKA patients’ and partners’ experiences regarding perspectives of sexual activity before and after surgery, complemented by the surgeons’ recommendations on safe resumption of sexual activity. More specifically, to examine whether certain sexual positions would be at risk for adverse outcomes (e.g., dislocation of the hip, insert luxation of the knee) and whether surgeons advise any safety measures.
The couples who participated estimated that they had resumed intercourse within three months after surgery. They adapted to new situations naturally. Before surgery, if necessary, they changed the leg position during sexual activity, while after surgery they resumed sexual activity as soon as they felt ready to have sex again. This finding was somewhat unexpected. In our previous studies, expectations on postoperative sexual activity were not met in up to 40% of THA and TKA patients, one year after surgery31,32. The cause and consequences of why expectations are not met are unknown. We thought that this might be related to functional difficulties with the prosthesis30, or the lack of knowledge about what to expect realistically11,30. Sexual dysfunction at older age is frequently reported7,16,40-42. Interestingly, our couples stated they were sexually active and did not experience any sexual dysfunction despite their age (range 55-73 years). Extensive literature pays attention to sexual dysfunction related to comorbidities43-48, However, our patients and most partners (except one) reported the presence of health issues and yet they did not report sexual dysfunction.
The limited available literature on sexual activity in THA and TKA patients have shown a preoperative reduction in sexual frequency12,27. In our study, only one couple had experienced decreased sexual frequency preoperatively, but did not express this as troublesome. The preoperative limitation of recreational activities and sport (e.g., long-distance hiking, hockey, traveling) was even more disappointing for most couples. In contrast, sexual activity was still present preoperatively, since it required less strenuous capacity, which possibly gave distraction from pain. One couple explicitly noted that despite OA, it was nice to experience that sex still was possible without pain. Some researchers hypothesized that oxytocin, which is released during intermate intimacy, may have a modulating effect on pain49,50. However, a review reported mixed results with regard to the association of oxytocin on emotional functioning and on the effect of pain reduction51.
The surgeons’ recommendations of safe sexual intercourse after THA have not been broadly discussed in the literature. In four countries (USA, UK, Switzerland and The Netherlands) expert opinions were gathered regarding safe sexual positions and the postoperative sexual “time out” for THA patients before resuming sexual activity26,33-35. However, no unanimous opinion was found. In our study, less than half of the THA surgeons, recommended a waiting time of 6 to 8 weeks (30-40%), probably keeping the estimated formation of the neo capsular tissue in mind52. Based on the surgeons' responses, no consistent view could be derived. Charbonnier and colleagues were the first who, based on virtual motion simulations, studied the relative risk of impingement and joint instability during 12 sexual positions. They took the mechanical relationships of the prosthetic parts into account. Charbonnier et al. particularly focused on the acetabular component, while leaving out the influence of muscles, ligaments, and capsules, and the femoral component. More detailed motion research is lacking. In our study, only 50% of the THA surgeons agreed with the findings of Charbonnier. The other half stated that there were no restrictions at all. As such, we did not get a uniform advice. Hence, more motions studies are necessary in order to develop national guidelines, that can be used to inform sexually active patients in a more consistent way. Until then, surgeons are advised to inform their patients about the lack of an expert opinion agreement, since it seems that patients are not always aware of the risks.
For TKA patients, surgeons agreed that there were no restrictions when resuming sexual intercourse. Surgeons had the opinion that after TKA kneeling or squatting could be inconvenient during some sexual positions (i.e., one position for men: position 3; and three positions for women: position 3, 10 and 11). Following a standard knee replacement, knee flexion usually is about 115 degrees (which always is less than a normal knee). Postoperative flexion is determined by the preoperative flexion, which is widely known in orthopedic research53. However, it is unclear if reduced flexion of the artificial knee has been recognized by patients as an important factor of impairment when regaining sexual activity after TKA. It is expected that couples will not be aware of limitations in these positions, until they experience unexpected discomfort during sex. This may be due to either the unexpected limited knee flexion and/or dysesthesia but also of the anterior knee scar. Thus, surgeons should inform their (sexually active) patients sufficiently and patients should expect moderate outcomes with respect to the decreased kneeling function after surgery29,30. Furthermore, women who expect to regain their preferred sexual position 10 and 11 postoperatively may be disappointed after surgery. Since some sexual positions require women to be able to deeply bend their knees, as deep bending of the knees will not be possible anymore53. Hence, explicit patient information is important, to prevent these unexpected limitations in positions and to manage expectations31,32. In our study, half of the surgeons felt no need to develop TKA patient information. We suggest that this is because there is still scant attention in literature on TKA patients’ sexual activity.
In the study of Wall, 12% of the partners felt fear of hurting their spouse26. Also, Yoon et al. published this finding11, whereas in our study, one partner experienced this fear of hurting his wife. When discussing safety measures during our interviews, couples became aware and felt that they would have liked to know more about when and how to resume sexual positions, which is in line with literature11-14,26,54. However, surgeons seem to avoid the subject34. Our couples did not understand why essential information about sex after surgery had not been provided by the surgeon. Written information should consist of practical information about (for TKA) uncomfortable and (for THA) permitted positions. This encourages "faithful trust" in surgeons and nurses55 and will foster an open communication culture.
Strengths and Limitations
Sexual activity is an important part of quality of life in THA and TKA patients24,56 and this study reveals that there is a gap between the patients’ and surgeons’ need of clear communication. The use of the 12 Dahm-drawings of sexual positions as tool to discuss with surgeons how they would advise patients and to ask couples about potential changes in their preferred sexual positions facilitated the discussion during the interviews and enhanced interpretation afterwards57,58. This pilot study can be seen as a first step in exploring qualitative issues of sexual activity in TKA and THA couples. Data saturation was achieved. All five couples gave the same narrative story and similar themes were distracted from the interviews.
This study has some limitations. Firstly, the interviews took place around 1.5 years after surgery. A correct reconstruction of the pre- and postoperative period was not always possible. Secondly, we interviewed a selective and small group of patients. The level of non-participation was high. All participating couples did not hesitate to talk about sexual activity. It could be that because of these attitude and communication skills, these couples were also better in coping and adapting to new circumstances naturally. This finding should be kept in mind when new qualitative research on sexuality is designed59,60. On the contrary, we invited couples to talk about sensitive topics. This could be an important reason for declining participation61. If we had chosen to interview patients without their partners, probably more persons would have been inclined to participate in this study. However, we were interested in the perspectives of sexually active couples. We realize that this choice gave us a selective group, resulting in selection bias. Due to the study design and eligibility criteria, important issues and perspectives of patients and partners may have been missed.
Conclusions
All couples physically and mentally adapted to the new situation and resumed sexual activity after surgery without considering or incorporating safety measures. Patients trusted their surgeons in their role as provider of necessary information. Thus, surgeons should be aware that patients expect their surgeon to inform them succinct about regaining sexual activity. This study emphasizes the importance of more explicit information on sexual activity during outpatient consultations. This will also add to more realistic patients’ expectations of sexual activity. The latter is even of more importance since the surgeons’ recommendations showed great variability. More motion research on hip and knee, may add to a more uniform postoperative advice after THA/TKA surgery.
Disclosure of Potential Conflicts of Interest
The institution or one or more of the authors (RTEH) has not received any funding for this study. Each author certifies that neither he or she, nor any member of his or her immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements) that might pose a conflict of interest in connection with the submitted article.
Ethical Review Committee Statement (formal letter is provided with the online version of the article) of University Medical Center Leiden, where the work was performed.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are submitted: forms are provided with the online version of the article.
Conflict of Interest
All authors stated they do not have a conflict of interest.
Acknowledgements
We thank the following surgeons: Orthopedic surgeons of the LOAS Study Group in the Netherlands: Dr. S. Verdegaal (Alrijne Hospital Leiderdorp) Dr. H. Kaptijn (Lange-Land Hospital, Zoetermeer), Dr. E van der Linden (Leids Universitair Medical Centre, Leiden) for their cooperation in sending the invitation letter and background information about the study to their patients and partners.
And in addition, the statistical support and cooperation of Professor Dr. Hein Putter from the department of Biomedical Data Sciences, Leiden University Medical Center, Leiden is highly appreciated, as well as the recommendations and contributing comments of Bart van der Zwan, professor of Vascular Neurosurgery at UMC Utrecht.
References
- Meiri R, Rosenbaum TY, Kalichman L. Sexual Function before and after Total Hip Replacement: Narrative Review. Sex Med. 2014; 2(4): 159-67.
- Keurentjes JC, Van Tol FR, Fiocco M, et al. Minimal clinically important differences in health-related quality of life after total hip or knee replacement: A systematic review. Bone Joint Res. 2012; 1(5): 71-7.
- Kurtz S, Mowat F, Ong K, et al. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005; 87(7): 1487-97.
- Grote S, Bürklein D, Kanz KG, et al. Hip prothesis and sexuality. What is when recommended? MMW Fortschr Med. 2008; 150(51-52): 44-5.
- Dutch Arthroplasty Register (LROI). Online LROI annual report 2019. Lroi [Internet]. 2019; (June): 57-62. Available from: https://www.lroi-rapportage.nl/
- Lindau ST, Gavrilova N. Sex, health, and years of sexually active life gained due to good health: evidence from two US population based cross sectional surveys of ageing. BMJ. Internatio. 2010; 340(9): 1-11.
- Tetley J, Lee DM, Nazroo J, et al. Let’s talk about sex - What do older men and women say about their sexual relations and sexual activities? A qualitative analysis of ELSA Wave 6 data. Ageing Soc. 2018.
- Gott M, Hinchliff S. How important is sex in later life? The views of older people. Soc Sci Med. 2003; 56(8): 1617-28.
- Hinchliff S, Tetley J, Lee D, et al. Older Adults’ Experiences of Sexual Difficulties: Qualitative Findings From the English Longitudinal Study on Ageing (ELSA). J Sex Res. 2018; 55(2): 152-63.
- Laupacis A, Bourne R, Rorabeck C, et al. The Effect of Elective Total Hip Replacement on Health-Related Quality of Life. Journal of Bone and Joint Surgery - Series A. 1993; 75(11): 1619-26.
- Yoon BH, Lee KH, Noh S, et al. Sexual Activity after Total Hip Replacement in Korean Patients: How They Do, What They Want, and How To Improve. Clin Orthop Surg. 2013; 5(4): 269-77.
- Nunley RM, Nam D, Bashyal RK, et al. The Impact of Total Joint Arthroplasty on Sexual Function in Young, Active Patients. J Arthroplasty. 2015; 30(2): 335-40.
- Stern SH, Fuchs MD, Ganz SB, et al. Sexual function after total hip arthroplasty. Clin Orthop Relat Res. 1991; 269: 228-35.
- Laffosse JM, Tricoire JL, Chiron P, et al. Sexual function before and after primary total hip arthroplasty. Joint Bone Spine. 2008; 75(2): 189-94.
- Lavernia CJ, Villa JM. High rates of interest in sex in patients with Hip arthritis. Clin Orthop Relat Res. 2015; 474(2): 293-9.
- Lindau ST, Schumm LP, Laumann EO, et al. A study of sexuality and health among older adults in the United States. N Engl J Med. 2007; 357(8): 762-74.
- Laumann EO, Paik A, Rosen RC. Sexual Dysfunction in the United States. JAMA: the journal of the American Medical Association. 2014; 281(6): 537-45.
- Traumer L, Jacobsen MH, Laursen BS. Patients’ experiences of sexuality as a taboo subject in the Danish healthcare system: a qualitative interview study. Scand J Caring Sci. 2019; 33(1): 57-66.
- Bell S, Reissing ED, Henry LA, et al. Sexual Activity After 60: A Systematic Review of Associated Factors. Sexual Medicine Reviews. 2017.
- Averyt JC, Nishimoto PW. Addressing sexual dysfunction in colorectal cancer survivorship care. J Gastrointest Oncol. 2014; 5(5): 388-94.
- van Ek GF, Krouwel EM, Nicolai MPJ, et al. Discussing Sexual Dysfunction with Chronic Kidney Disease Patients: Practice Patterns in the Office of the Nephrologist Discussing Sexual Dysfunction with Chronic Kidney Disease. Journal of Sexual Medicine. 2015; 12: 2350-63.
- Nicolai MPJ, Fidder HH, Beck JJH, et al. Sexual Abuse History in GI Illness, How Do Gastroenterologists Deal with It? Journal of Sexual Medicine. 2012; 9(5): 1277-84.
- Krouwel EM, Albers LF, Nicolai MPJ, et al. Discussing Sexual Health in the Medical Oncologist’s Practice: Exploring Current Practice and Challenges. Journal of Cancer Education. 2020; 35(6): 1072-88.
- Harmsen RThE, Haanstra TM, Sierevelt IN, et al. Does total hip replacement affect sexual quality of life? BMC Musculoskelet Disord. 2016; 198(1): 17.
- Currey HLF. Osteoarthrosis of the hip joint and sexual activity. Ann Rheum Dis. 1970; 29(5): 488-93.
- Wall PDH, Hossain M, Ganapathi M, et al. Sexual activity and total hip arthroplasty: a survey of patients’ and surgeons’ perspectives. Hip Int. 2011; 21(2): 199-205.
- Wang BL, Yue DB, Liu BX, et al. Quality of sexual life after total hip arthroplasty in male patients with osteonecrosis of femoral head. Eur J Orthop Surg Traumatol. 2014; 24(7): 1217-21.
- Meyer H, Stern R, Fusetti C, et al. Sexual quality-of-life after hip surgery - Springer. Journal of Orthopaedics and Traumatology. 2003; 4(1): 21-5.
- Klit J, Jacobsen S, Sonne-Holm S, et al. Arthrosis and arthroplastic surgery influence patients’ sex life, depression, and socioeconomy. Ugeskr Laeger [Internet]. 2011 [cited 2014 Feb 13]; 173(21): 1499-502. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21627913
- Kazarian GS, Lonner JH, Hozack WJ, et al. Improvements in Sexual Activity After Total Knee Arthroplasty. J Arthroplasty. 2017; 32(4): 1159-63.
- Harmsen RThE, Den Oudsten BL, Putter H, et al. Patient Expectations of Sexual Activity After Total Hip Arthroplasty. J Bone Joint Surg open acces. 2018; 0(e0031): 1-9.
- Harmsen RTE, Haanstra TM, Oudsten BL Den, et al. A High Proportion of Patients Have Unfulfilled Sexual Expectations After TKA: A Prospective Study. Clin Orthop Relat Res. 2019; 478(9): 1-13.
- Dahm DL, Jacofsky D, Lewallen DG. Surgeons Rarely Discuss Sexual Activity with Patients after THA; A survey of members of the American Association of Hip and Knee Surgeons. Clin Orthop Relat Res. 2004; 428(428): 237-40.
- Harmsen RThE, Nicolai MPJ, Den Oudsten BL, et al. Patient sexual function and hip replacement surgery: A survey of surgeon attitudes. Int Orthop. 2017.
- Charbonnier C, Chagué S, Ponzoni M, et al. Sexual Activity After Total Hip Arthroplasty: A Motion Capture Study. J Arthroplasty [Internet]. 2014; 29(3): 640-7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24018159
- Leichtenberg CS, Meesters JJL, Kroon HM, et al. No associations between self-reported knee joint instability and radiographic features in knee osteoarthritis patients prior to Total Knee Arthroplasty: A cross-sectional analysis of the Longitudinal Leiden Orthopaedics Outcomes of Osteo-Arthritis study. Knee. 2017; 24(4): 816-23.
- McCabe MP, Sharlip ID, Lewis R, et al. Risk Factors for Sexual Dysfunction Among Women and Men: A Consensus Statement From the Fourth International Consultation on Sexual Medicine 2015. Journal of Sexual Medicine. 2016; 13(2): 153-67.
- Miles Matthew B, Huberman MA. Qualitative data analysis. Higher Education Research Methodology. 2018.
- Johnson JK, Barach P, Vernooij-Dassen M. Conducting a multicentre and multinational qualitative study on patient transitions. BMJ Qual Saf. 2012; 21(SUPPL. 1): 22-8.
- Beckman N, Waern M, Östling S, et al. Determinants of sexual activity in four birth cohorts of Swedish 70-year-olds examined 1971-2001. Journal of Sexual Medicine. 2014.
- Beckman N, Waern M, Gustafson D, et al. Secular trends in self reported sexual activity and satisfaction in Swedish 70 year olds: cross sectional survey of four populations, 1971-2001. Bmj. 2008; 337(jul08 3): a279-a279.
- Wright H, Jenks RA. Sex on the brain! Associations between sexual activity and cognitive function in older age. Age Ageing. 2016.
- Berlo Willy, Vennix P, Rasker JJ, et al. Rheumatic diseases and sexuality: a review of the literature. Rheumatology Europe. 1999; 28(3): 113-7.
- Nicolai MPJ, Elzevier HW. Do residents in cardiology need more training to make them talk about sex? Netherlands Heart Journal. 2014; 22(3): 122-3.
- van Berlo, Willy T M, van der Wiel Harry BM, et al. Sexual functioning of people with rheumatoid arthritis: a multicenter study. Clin Rheumatol. 2007; 26(1): 30-8.
- Palmer D, El Miedany Y. Sexual dysfunction in rheumatoid arthritis: a hot but sensitive issue. Br J Nurs. 20(17): 1134-7.
- El Miedany Y, El Gaafary M, El Aroussy N, et al. Sexual dysfunction in rheumatoid arthritis patients: arthritis and beyond. Clin Rheumatol. 2012; 31(4): 601-6.
- Nicolai MPJ, Liem SS, Both S, et al. What do cardiologists know about the effects of cardiovascular agents on sexual function? A survey among Dutch cardiologists. Part I. Netherlands Heart Journal. 2013; 21(12): 540-4.
- Jurek B, Meyer M. Anxiolytic and Anxiogenic? How the Transcription Factor MEF2 Might Explain the Manifold Behavioral Effects of Oxytocin. Front Endocrinol (Lausanne). 2020; 11: 2020.
- Baettig L, Baeumelt A, Ernst J, et al. The awareness of the scared - context dependent influence of oxytocin on brain function. Zurich Open Repository and Archive. 2020; 14: 2073-83.
- Mekhael AA, Bent JE, Fawcett JM, et al. Evaluating the Efficacy of Oxytocin for Pain Management: An Updated Systematic Review and Meta-Analysis of Randomized Clinical Trials and Observational Studies. Canadian Journal of Pain. 2023; 7(1): 1-19.
- Van Der Weegen W, Kornuijt A, Das D. Do lifestyle restrictions and precautions prevent dislocation after total hip arthroplasty? A systematic review and meta-analysis of the literature. Clin Rehabil. 2015; 30(4): 329-39.
- Nelissen RGHH. Fundamental aspects of the clinical evaluation of total joint prostheses: the total condylar knee prosthesis [Internet]. S.l.: s.n.]; 1995 [cited 2023 Jun 12]. Available from: https://catalogue.leidenuniv.nl/primo-explore/fulldisplay?docid=UBL_ALMA21160430140002711&context=L&vid=UBL_V1&lang=en_US&search_scope=All_Content&adaptor=Local%20Search%20Engine&tab=all_content&query=any,contains,fundamental%20aspects%20nelissen
- Klit J, Jacobsen S, Schmiegelow V, et al. Results of total joint arthroplasty and joint preserving surgery in younger patients evaluated by alternative outcome measures. Dan Med J. 2014; 61(4): 1-19.
- Brodney S, Sepucha K, Chang Y, et al. Patients Who Reviewed a Decision Aid Prior to Major Orthopaedic Surgery Reported Higher Trust in Their Surgeon. JBJS Open Access. 2022.
- World Health Organization W group, Working-group W. Defining sexual health: Report of a technical consultation on sexual health, Geneva. Geneva: World Health Organization; 2002.
- Kallio H, Pietilä AM, Johnson M, et al. Systematic methodological review: developing a framework for a qualitative semi-structured interview guide. J Adv Nurs. 2016; 72(12): 2954-65.
- Turner DW. Qualitative interview design: A practical guide for novice investigators. Qualitative Report. 2010; 15(3): 754-60.
- Dunne MP, Martin NG, Michael Bailey J, et al. Participation bias in a sexuality survey: Psychological and behavioural characteristics of responders and non-responders. Int J Epidemiol. 1997; 26(4): 844-54.
- Strassberg DS, Lowe K. Volunteer bias in sexuality research. Arch Sex Behav. 1995; 24(4): 369-82.
- Coleman LM, Ingham R. Exploring young people’s difficulties in talking about contraception: How can we encourage more discussion between partners? Health Educ Res. 1999; 14(6): 741-50.
Additional File: Interview Guide
|
Objectives |
Questions used in the semi structured interview |
|
Research objective 1 To explore what having "a worn hip/knee" means for the sex life of patients and their partners. |
For the patient: As a starting question, - Can you tell us what it was like for you to live with "a worn hip/knee"? How long did that phase last before you had surgery (number of months/years)? - Can you indicate (and express) how healthy you feel today (EQ5D VAS 0-100)? - Can you tell me what it is like to live with a prosthesis (possibly what about the pain and functioning in daily life)? Measurement of the result of your surgery? (VAS 0-100) For the partner: - What did it mean to you, to live with a partner who had a worn out hip/knee? For both: - Can you tell us something about the proces of staying sexually active (intercourse) until surgery and after that? If no longer sexually active: Can you tell us something about why you stopped having intercourse? What is the influence of the degenerative hip/knee? - Can you tell something about the influence of age; health complaints, joy in life etc.? (For the partner: if sexual intercourse stopped, what did this mean to you?) |
|
|
If remained sexually active: - Looking back at the time of the 'degenerative hip/knee' and the moments of intercourse, can you tell something about how that functioned? For both: - If you both look back, can you remember how often you had intercourse? Can you indicate whether this was less than before OA started (What was your "normal pattern" when you did not have a worn hip/knee?) - Can you recall what a worn hip/knee does to developing a desire for sex? - Looking back, to what extent did sex (quality of intercourse) with a worn hip/knee play a role in getting the surgery (faster)? Is there anything from that period of "worn hip/knee" and "sex" that is important to recount? |
|
Research objective 2 To explore what having a prosthesis (hip/knee) means for the sex life of patients and their partners |
- Can you say anything about how it went the first time with the new hip/knee? How soon after surgery (number/month week)? Can you tell us something about the influence a new hip or knee has on the desire for sex? To what extent has sex improved after the operation? For the partner: - What did it mean for you to have intercourse with your partner who has a hip/knee replacement? For all patients (active and not active) - Can you say something about whether you both have deteriorated in health in the last year? Could you tell us something about the lust for sex during rehabilitation; Can you say something about the comparison with the past? Can you say something about the influence of time (age) on your sex life (intercourse)? Can you say something about whether your sexual relationship has changed because of hip/knee surgery? Can you say something about how important having intercourse is to you? |
|
Research objective 3 To explore if there is a change in the (preferred) sexual positions |
Questions for both - Which position(s) do you prefer? (use drawings to point out); before and after surgery. - Can you tell something about your choice; If they have changed, why? - If the favorite position is no longer possible, what does this mean and why can't you do it? How does that affect you? Were there other reasons why you have changed your favorite position? - Can you tell us something about your thoughts and feelings of being safe during intercourse? And about your expectations on that point? |
|
To explore the moment of resuming intercourse |
- When exactly did you think you were ready for engaging in sexual intercourse? (number of weeks/months after the operation); Can you tell us what that moment was based on? |
|
Research objective 4 To explore the need for communication, information and/or instruction |
- Regarding the need for information: Can you tell what you would like to know, to feel well informed and prepared? And what role do you see for yourself and or your partner to ask for? What information do you need as a partner? Providing information by whom? Can you tell something about the need for instruction e.g., for the leg position? |
