Multiple Diagnoses of Nutritional Rickets in An Inner-City Pediatric Population: A Case Series
Michelle Jeffery1, Judy-Mae Lima2, Aditi Khokhar3, O. Folorunsho Edobor-Osula2*
1Rutgers Robert Wood Johnson Medical School, Piscataway, NJ, USA
2Department of Orthopaedic Surgery, Rutgers New Jersey Medical School, Newark, NJ, USA
3Pediatric Endocrinology, Goryeb Children’s Hospital, Morristown, NJ, USA
Abstract
This case series details seven pediatric cases of nutritional rickets in an inner-city population of New Jersey. Eighty six percent of these patients were exclusively breast fed, and all self-identified as black or African American. Patients ranged in age from 8 months to 3 years at the time of initial diagnosis. All seven patients were male. Five patients were presented in an office setting, while two were found to have nutritional rickets in an emergency setting. Patients demonstrated classic pathognomonic findings of rickets, including three patients with rachitic rosary. The aim of this case series is to emphasize the importance of surveillance and high clinical suspicion for nutritional rickets, particularly in children with darker skin complexions and who were exclusively breast-fed during infancy. Rapid diagnosis and intervention may delay or negate the need for orthopedic surgical intervention.
Introduction & Literature Review
Nutritional rickets is defined as a defective mineralization of bone, particularly in the growth plates and osteoid matrix, often due to vitamin D deficiency, hypocalcemia, or metabolism of these nutrients1. The global incidence of nutritional rickets is rising, even in the United States and other high-income countries2. Nutritional rickets had largely disappeared from industrialized countries when food fortifications programs were introduced, but there has been a re-emergence over the past two decades1. In the US alone, the prevalence of rickets has increased from 0 per 100,000 in 1970 to 3.7 per 100,000 in 1990, and further up to 24.1 per 100,000 in 20001. Although there is a paucity of data on the incidence of this diagnosis in the US alone, the case rate is predicted to be 2.9-27 per 100,000 individuals in the US and Europe as of 20213.
The prevalence of nutritional rickets is several hundred-fold higher in dark-skinned populations when compared to light-skinned populations2. In fact, the likelihood of vitamin D deficiency can range anywhere from 3x-71x higher in these individuals2. General risk factors for nutritional rickets include dark skin pigment, children under the age of three who were exclusively breast fed, and low exposure to sunlight4.
While several recent case reports have been published5-9, most recently in 2023 in the United States, nutritional rickets in infants can be overlooked due to many nonspecific clinical manifestations2. Recent case reports have been seen from Morocco and remote regions of Myanmar, but to our knowledge, no recent case studies of nutritional rickets have been reported in the United States5-8. This case series will review seven documented cases of nutritional rickets seen at an inner-city university hospital in New Jersey. For the sake of brevity, details such as past medical history, family history, social history, etc. are noncontributory if not otherwise noted in the case, and only notable physical exam findings are listed.
Case 1
A 3-year-old male presented for evaluation of persistent genu varum. His parents noted frequent tripping, especially when compared to peers. The patient was born full term via vaginal delivery with no complications. He was exclusively breastfed for two months, after which time he was switched to formula feeding. Since starting solid food, he consumed a normal diet with dairy products. He began walking at 11 months. The patient was 5%ile in height and 34%ile in weight.
On gait exam, the bilateral legs displayed significant genu varum at baseline. The patient had an intoeing gait with genu varum on the right greater than left. Bilateral tibia/fibula series and a mechanical axis series were obtained. XR tib-fib demonstrated rickets with resultant bowing deformities, and noted cupping and fraying of the metaphysis at the knee and ankle. Mechanical axis showed bilateral genu varum with 4.5cm medial mechanical deviation on the right and 3.7cm deviation on the left. (Figure 1). Laboratory results are included in Table 1 and are consistent with a diagnosis of nutritional rickets.
Upon referral to Pediatric Endocrinology, the patient was started on calcium carbonate 5mL PO TID (total 1,250mg) and vitamin D (4,000 units daily) with some improvement in clinical presentation. At the first follow up visit, he was fit for bilateral HKAFOs orthotics. Subsequent follow up demonstrated he was tolerating his orthoses well, with further improvement in the bowing of the right leg.
Several months after his initial evaluation, he presented with a right supracondylar humerus (SCH) fracture after a fall. His physical exam demonstrated swelling and tenderness to palpation at the elbow, with limited range of motion due to pain. He was placed in a long arm cast, which was removed 1 month later. At that time, repeat imaging showed a healing right SCH fracture. His mother reported running out of calcium carbonate, and as a result the patient had not received therapeutic dosing in approximately 9 months. Physical exam remained unchanged, and his mother was counseled on the importance of nutrition and its’ relation to bone and overall health. The underlying pathophysiology of his vitamin D and calcium deficiency was not readily apparent.
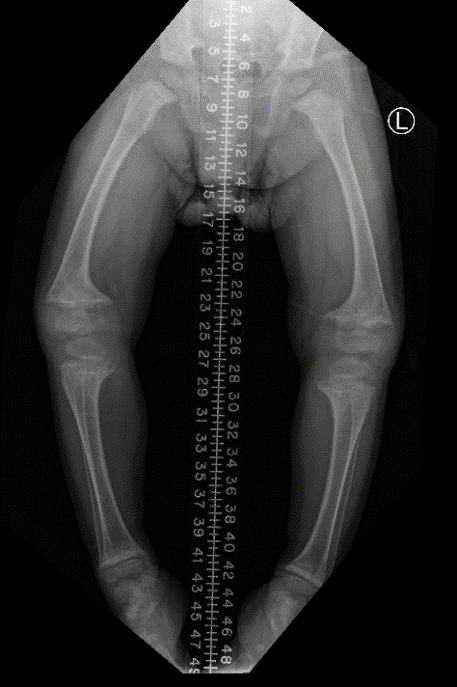
Figure 1: Case #1 (Mechanical Axis XR) AP
Table 1: Case #1 Lab Values
|
Timeline of therapeutic dosing |
Calcium (mg/dL) |
Phosphorus (mg/dL) |
25 OH-Vitamin D (ng/ mL) |
PTH (pg/ mL) |
Alkaline Phosphatase(u/L) |
Calcitriol (1,25 DI-OH VIT D) (pg/ mL) |
|
Month 0 |
6.2* |
3.8 |
<3.4* |
448 |
1,837 |
60.8 |
|
Month 0.5 |
7.6** |
3.5 |
- |
- |
- |
- |
|
Month 1 |
9.4** |
4.5 |
11.9** |
136 |
1,067 |
- |
Month 0 = baseline before therapeutic dosing, *: prior to therapeutic dosing, **: after therapeutic dosing
Case 2
A 2-year-old male was sent to the ED by his pediatrician given concern for failure to thrive and possible rickets. In the ED, he was found to have severe hypocalcemia, poor growth, delayed motor development, and multiple fractures. The skeletal survey in the ED showed advanced rickets with multiple fractures, including a non-displaced right distal radius and ulna fracture, bilateral non-displaced fibula fractures, and delayed ossification. Additionally, there was diffusely poor mineralization of multiple bones on x-ray of the skull, chest, pelvis, bilateral femurs, thoracic and lumbar spine. There was prominence to the anterior ribs (rachitic rosary), cupping and fraying of metaphyses of the femurs, humeri, and bones of the forearm bilaterally, with dorsal bowing deformity of both radius and ulna (Figure 2-3).
The patient was then admitted to the PICU from the ED for IV calcium and the need for telemetry. Of note, The Division of Child Protection and Permanency was called for concerns regarding medical neglect, given the severity of his symptoms and the lack of follow up with the pediatrician since birth. Upon taking additional history from his mother, she stated he was mostly breastfed, with very little solid food intake up until that point. She had noticed a delay in walking but had not sought evaluation. The patient was discharged on therapeutic treatment with calcium carbonate (600mg TID), vitamin D (4000 units qd), and multivitamins.
The patient presented to the outpatient orthopedic surgery clinic 5 months after his initial hospitalization for rickets. His mother reported he was now crawling at home and nearly walking. On exam in this outpatient setting, the patient was crawling around the exam table comfortably. The patient was <1%ile weight, <1%ile length, and 10%ile in height. He demonstrated a prominent kyphotic thoracic spine, widened wrists, and rachitic rosary. Laboratory results are included in Table 2. The patient was instructed to follow up after he began ambulating with repeat radiographs at that time.

Figure 2: Case #2 (CXR) AP

Figure 3: Case #2 (L femur XR) lateral
Table 2: Case #2 Lab Values
|
Timeline of therapeutic dosing |
Calcium (mg/dL) |
Phosphorus (mg/dL) |
25 OH-Vitamin D (ng/ mL)
|
PTH (pg/ mL)
|
Alkaline Phosphatase(u/L)
|
Calcitriol (1,25 DI-OH VIT D) (pg/ mL) |
|
Week 0 |
-* |
- |
5.1* |
192 |
- |
- |
|
Week 0.5 |
7.3** |
- |
5.1** |
192 |
- |
- |
|
Week 1 |
8.3 |
2.3 |
- |
- |
- |
- |
|
Week 3 |
8.4 |
2.0 |
20.2 |
158 |
3,316 |
966 |
|
Month 2 |
9.1 |
2.8 |
18.7 |
116 |
2,101 |
- |
|
Month 4 |
9.0 |
4.0 |
25.4 |
97 |
881 |
- |
|
Month 7 |
9.2 |
- |
85.4 |
- |
538 |
- |
|
Month 12 |
9.1 |
- |
16.6 |
- |
431 |
- |
Month 0 = baseline before therapeutic dosing, *: prior to therapeutic dosing, **: after therapeutic dosing
Case 3
An 8-month-old male presented to an outpatient orthopedic surgery clinic after a displaced transverse fracture of the shaft of the left femur. He was initially seen in the ED one week prior, after his parents noticed a lack of left lower extremity movement. X-rays and metabolic panels demonstrated calcipenic nutritional rickets. The patient was exclusively breast fed with no supplementation. He was not taking any medications at the time of presentation, but was started on therapeutic vitamin D after discharge from the ED. On exam he had an intact one-legged spica cast on the left with no wounds or ulcerations. He was <1%ile in height. XR of left femur showed a minimally displaced fracture through the midshaft of the left femur. The overlying cast obscured fine bony detail (Figure 4). Laboratory results are included in Table 3. The patient was instructed to follow up with repeat imaging in 2 weeks. After cast removal, repeat radiographs showed a well healed fracture. His mother was counseled on the need for continued observation for femoral overgrowth, with no further documentation available after this visit.

Figure 4: Case #3 (L femur XR) AP
Table 3: Case #3 Lab Values
|
Timeline of therapeutic dosing |
Calcium (mg/dL) |
Phosphorus (mg/dL) |
25 OH-Vitamin D (ng/ mL) |
PTH (pg/ mL) |
Alkaline Phosphatase(u/L) |
Calcitriol (1,25 DI-OH VIT D) (pg/ mL) |
|
Week -3 |
6.3* |
2.5 |
8* |
653 |
1,461 |
- |
|
Month 1 |
10.5** |
4.8 |
16.5** |
41 |
864 |
563.4 |
Month 0 = baseline before therapeutic dosing, *: prior to therapeutic dosing, **: after therapeutic dosing
Case 4
A 16-month-old male was referred by his pediatrician for a delay in walking. The patient was able to pull to stand but would not take assisted steps. He started crawling at 12 months, but his parents felt it looked notably different than peers. The patient was reaching all other developmental milestones. The patient was breast fed until 4.5 months when solids were introduced. He had never been bottle fed, did not drink milk, and never received vitamin D supplementation. The patient was born at full term with a normal vaginal delivery. His past medical history notable for eczema and multiple food allergies (eggs, dairy, peanuts, wheat).
On exam, the patient did not ambulate. There was a palpable rachitic rosary along the ribs. There was no significant bowing of the tibia and no leg length discrepancy. Hip abduction was full and symmetric. X-ray imaging showed profoundly demineralized bone, cupping and fraying of the epiphyses and periosteal new bone formation along the distal ulnar shaft with mild bowing deformity (Figure 5). This impression led to a radiographic diagnosis of advanced rickets. Laboratory results are included in Table 4. The patient was referred to Endocrinology and started on Calcium carbonate 2.6mL PO qAM (650mg total) and multivitamins. After a few months of treatment, he began walking independently and was gaining strength. At 6 month follow up, he was running and reaching all other developmental milestones. Repeat XR demonstrated improving osseous mineralization and almost complete resolution of previously seen rachitic changes. At that time, he was cleared from an orthopedic standpoint but continued to follow with Endocrinology.

Figure 5: Case #4 (L wrist XR) AP
Table 4: Case #4 Lab Values
|
Timeline of therapeutic dosing |
Calcium (mg/dL) |
Phosphorus (mg/dL) |
25 OH-Vitamin D (ng/ mL) |
PTH (pg/ mL)
|
Alkaline Phosphatase(u/L)
|
Calcitriol (1,25 DI-OH VIT D) (pg/ mL) |
|
Month 0 |
6.1* |
2.7 |
<3.4* |
340 |
2,632 |
563.4 |
|
Month 0.5 |
7.4** |
2.8 |
24.9** |
- |
2,328 |
- |
|
Month 1 |
- |
3.1 |
31.2 |
- |
2,710 |
- |
|
Month 3 |
- |
4.6 |
34.3 |
- |
1,471 |
564 |
|
Month 6 |
9.8 |
5.5 |
35.7 |
77 |
292 |
283.2 |
|
Month 8 |
9.9 |
3.6 |
31.9 |
25 |
357 |
105 |
Month 0 = baseline before therapeutic dosing, *: prior to therapeutic dosing, **: after therapeutic dosing
Case 5
A 9-month-old male was initially referred for evaluation after concerning pelvic XR at an outside hospital. These images were not readily available. His mother denied evidence of pain and had no concerns about his hips prior to evaluation. The patient had met all developmental milestones appropriately. He sat and crawled by 5 months. The patient was mostly breastfed and was reportedly a “picky eater” with regular table food. He did not receive supplementation with whole milk but was given a multivitamin that contained vitamin D. There was questionable lead exposure in the home. He was born at full term with the pregnancy complicated by gestational HTN.
On exam, there was a birthmark noticed on the skin overlying the proximal spine. There was mild widening of the bilateral wrists and repeat XR was recommended in 3 months. Laboratory results are included in Table 5. There was no acute intervention at that time.
At his follow up at 12-months of age, his mother noted the patient began to pull to stand at 10 months and walked independently at 11 months old. On examination, the patient was able to stand with assistance but demonstrated new bowed leg deformities bilaterally. On physical exam, leg lengths were equal, with bilateral bowing deformity and tibial torsion. There was an extra right thigh crease and significantly palpable rachitic rosary sign. Imaging at this visit showed expansion of the distal radius physes and ulna physes of both the right and left wrist (Figure 6). There was typical “cupping” and sclerosis with demineralization findings associated with rickets. Additionally, there was mild right hip dysplasia, with diminished mineralization of the right femoral head when compared to the left. The patient’s mother was educated on the clinical and radiograph findings, with immediate referral to Endocrinology for evaluation. At that Endocrinology visit, the patient was found to have low vitamin D levels, so therapeutic vitamin D and solid food intake were recommended as a result. There is no documentation detailing additional intervention or treatment following that visit.
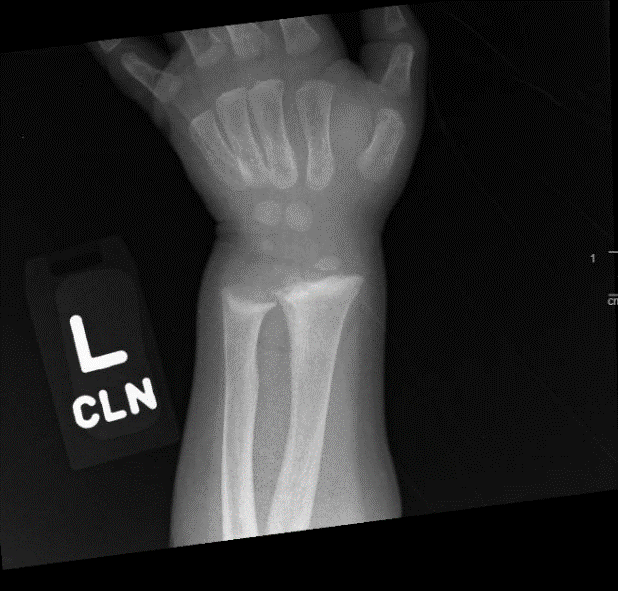
Figure 6: Case #5 (L wrist XR) AP
Table 5: Case #5 Lab Values
|
Timeline of therapeutic dosing |
Calcium (mg/dL) |
Phosphorus (mg/dL) |
25 OH-Vitamin D (ng/ mL)
|
PTH (pg/ mL)
|
Alkaline Phosphatase(u/L)
|
Calcitriol (1,25 DI-OH VIT D) (pg/ mL) |
|
Month 7 |
9.9 |
5.0 |
14.1** |
137 |
1,016 |
279.3 |
Month 0 = baseline before therapeutic dosing, *: prior to therapeutic dosing, **: after therapeutic dosing
Case 6
A 16-month-old male was referred by his pediatrician for evaluation of bilateral varus deformities of the lower extremities. This was first noticed when he began bearing weight, but per his mother this had not caused any concerns with ambulation. The patient had been exclusively breast fed since birth with no supplementation and only documentation of consuming a “balanced diet” once he reached 23 months of age. It is unclear if he consumed solid food prior to this time. The patient was born at full term with a normal vaginal delivery.
On gait exam, he had a normal stance phase with in-toeing. There was apparent varus deformity of both the femur and tibia while bearing weight. On imaging, the right lower extremity measured 31.7cm in length, while the left measured 33.2m in length. Morphologic changes of both proximal tibia metaphyses were noted (Figure 7).
The patient was sent to the pediatrician to obtain a vitamin D level and instructed to return in 6 months for repeat radiographs. This laboratory analysis was performed at an OSH and records are not currently available. However, eight months after initial presentation the patient had started on therapeutic vitamin D with notable improvement in the bowing of his legs, and was presumed to be treated for nutritional rickets secondary to vitamin D deficiency. On repeat exam, he had a normal stance phase and foot progression angle with an intoeing gait. Repeat imaging demonstrated a lower extremity length of 37.9cm on the right and 37.7cm on the left, with morphologic changes of both proximal tibia metaphyses. The patient was fit for bilateral KAFOs, with consideration of surgical intervention by age 4 years if no improvement was noted.
The patient was seen 7 months later at the age of 22 months, at which time he was no longer taking therapeutic vitamin D and was eating a balanced diet. Post-treatment lab values are included in Table 6. He tolerated orthoses without concern. Imaging demonstrated persistent lateral bowing of the femur and tibia bilaterally. There was normal bone density, and only mild widening of the distal femoral physes bilaterally, read as “Findings may be sequalae of treated rickets”. Though the aforementioned findings, including significant improvement post-vitamin D dosing, are highly suggestive of nutritional rickets, the vitamin D levels taken at the outside facility were not available, so a definitive diagnosis of nutritional rickets cannot be made. At that time, he was referred to Endocrinology for further workup, with repeat SMA films in 3 months.

Figure 7: Case #6 (Mechanical axis XR) AP
Table 6: Case #6 Lab Values
|
Timeline of therapeutic dosing |
Calcium (mg/dL) |
Phosphorus (mg/dL) |
25 OH-Vitamin D (ng/ mL)
|
PTH (pg/ mL)
|
Alkaline Phosphatase(u/L)
|
Calcitriol (1,25 DI-OH VIT D) (pg/ mL) |
|
Month 6 |
10.2 |
5.5 |
82.2** |
24 |
267 |
53.8 |
Month 0 = baseline before therapeutic dosing, *: prior to therapeutic dosing, **: after therapeutic dosing
Case 7
A 2-year-old male, with a history of failure to thrive (FTT) of unknown cause was referred to Endocrinology after initial workup of FTT showed high alkaline phosphatase levels. The patient was 2690g at birth, with poor weight gain and growth in the first year of life, with growth curve trajectories worsening over time. On further evaluation, he had extremely low vitamin D and a high PTH level, and was initially started on Vitamin D 4000 units PO qd and CaCO3 625mg BID. When presenting to the outpatient orthopedic office, he had since decreased Vitamin D to 1000 units PO qd and CaCO3 625mg qd, with notable improvement in growth. Per his mother, he was also running and walking without difficulty, with no bowing of the legs. Family history was notable for mother and maternal uncle with rickets during childhood.
On physical exam, he was 7%ile in height and 5%ile in length. The patient exhibited a normal gait with no leg bowing and normal muscle tone. XR of the bilateral wrists showed diffuse demineralization with periosteal new bone formation noted along all metacarpal bones and to a lesser degree at the radius bilaterally. There was some bowing deformity of the radius bilaterally. Additionally, there was cupping and fraying of the metaphyses with markedly widened growth plates. XR of the bilateral tib-fib also showed profound and diffuse demineralization with bowing deformities of the tibia and fibular shafts bilaterally (Figure 8). There was cupping and fraying of the metaphyses and markedly widened growth plates bilaterally, consistent with advanced rickets. Laboratory results are included in Table 7.
Repeat radiographs five months after his first orthopedic visit showed significant improvement in bone mineralization and endochondral ossification, compatible with treated rickets. Biochemical and XR findings have been progressively improving with therapeutic Vitamin D and calcium, suggesting nutritional rickets as the underlying etiology. The patient was instructed to continue Vitamin D at 1000 units qd, but discontinued CaCO3.
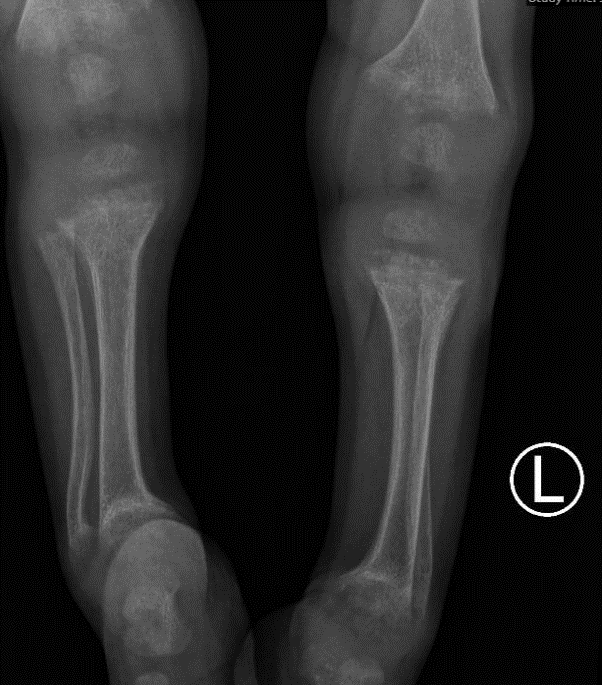
Figure 8: Case #7 (bilateral tibia/fibula XR) AP
Table 7: Case #7 Lab Values
|
Timeline of therapeutic dosing |
Calcium (mg/dL) |
Phosphorus (mg/dL) |
25 OH-Vitamin D (ng/ mL)
|
PTH (pg/ mL)
|
Alkaline Phosphatase(u/L)
|
Calcitriol (1,25 DI-OH VIT D) (pg/ mL) |
|
Month -2 |
9.0 |
- |
- |
- |
2,819 |
- |
|
Month -1 |
9.5 |
2.4 |
5.7 |
- |
2575 |
- |
|
Month 0 |
8.9 |
2.4 |
4.4* |
340 |
2,688 |
- |
|
Month 1 |
9.2 |
4.1 |
21.2** |
- |
2,290 |
666 |
|
Month 2 |
9.4 |
- |
17.3 |
121 |
1,830 |
549 |
|
Month 5 |
9.8 |
6.2 |
19.4 |
36 |
526 |
330 |
|
Month 6 |
10.2 |
5.8 |
16.7 |
24 |
492 |
- |
|
Month 9 |
9.2 |
6.4 |
14.9 |
- |
495 |
- |
|
Month 10 |
10.1 |
- |
34.9 |
- |
407 |
- |
|
Month 15 |
10.5 |
5.8 |
42.6 |
22 |
338 |
- |
|
Month 19 |
- |
- |
24.3 |
- |
342 |
- |
|
Month 19.8 |
9.4 |
- |
13.4 |
30 |
336 |
- |
Month 0 = baseline before therapeutic dosing, *: prior to therapeutic dosing, **: after therapeutic dosing
Case Summaries
Though all unique, the aforementioned case studies have notable similarities (Table 8). Five patients had initial evaluations in an outpatient orthopedic clinic while two were found to have nutritional rickets in an emergency setting. For those seen in the outpatient office, all presented for evaluation of gait abnormalities and were often referred by pediatricians. Those seen in the ED were likely to present with a fracture or other sequelae and subsequently found to have abnormal laboratory values on further workup. Only one patient had a known family history of rickets. Similarly, all but one patient had no known medical history at the time of presentation. Most notably, 85.7% of the patients were exclusively breastfed for some period of time during infancy, and all self-identified as black or African American.
Clinically, a majority of patients were less than 10%ile in height (n=4), with 2 patients ≤10%ile in weight. Radiographic evidence of rickets was seen via cupping and fraying of metaphyses, demineralization, and bowing of the long bones. Three patients exhibited the classic rachitic rosary, which is nearly pathognomonic of rickets.
At the time of presentation, four patients exhibited low calcium (ranging from 6.1-7.3 mg/dl) and six exhibited low vitamin D (ranging from <3.4-14.1 ng/mL). Patients also demonstrated elevations in alkaline phosphatase (ranging from 864-2,632 u/L), calcitriol (1,25 DI-OH VIT D) (ranging from 279.3-563.4 pg/mL), and PTH (ranging from 137-448 pg/mL). Patients who were started on therapeutic calcium carbonate and vitamin D exhibited not only a clinical improvement (meeting developmental milestones, etc.), but also an objective improvement in osseous mineralization as visualized on radiographs and objective improvements in lab values. When multiple data points were available, all values either returned to expected range or were trending appropriately. Several patients even demonstrated complete clinical resolution of nutritional rickets without surgical intervention and were discharged from an orthopedic standpoint.
Table 8: Summary of Cases
|
Case # |
Age |
Sex (M/F) |
Clinical signs / symptoms |
Location of initial presentation |
History of exclusive breast feeding (Y/N) |
Prior vitamin D supplementation |
Height/ Weight %ile
|
|
1 |
3 years |
M |
Genu varum since birth, frequent tripping |
Orthopedic Outpatient |
Y |
N |
5% height, 34% weight |
|
2 |
2 years |
M |
FFT, curvature in back, b/l wrist widening, severe hypocalcemia |
Emergency department
|
Y |
N |
<1% height 10% weight |
|
3 |
8 m.o. |
M |
Femoral shaft fx |
Emergency department |
Y |
N |
<1% height 65% weight |
|
4 |
16 m.o |
M |
Delayed walking |
Orthopedic Outpatient |
Y |
N |
15% height 84% weight |
|
5 |
9 m.o |
M |
Possible hip deformity |
Orthopedic Outpatient |
Y |
Y |
23% height 75% weight |
|
6 |
16 m.o |
M |
Bilateral varus deformity |
Orthopedic Outpatient |
Y |
N |
96% height >99 weight |
|
7 |
2 years |
M |
Failure to thrive |
Endocrinology Outpatient |
N |
N |
7% height 5% weight |
Reference ranges: (Table 1-8)
- Calcium: (9.0 - 11.0 mg/dl)
- Phosphorus: (4.5 - 6.5 mg/dl)
- Magnesium: (1.6 – 2.6 mg/dl)
- 25 OH-Vitamin D: (>30 ng/ mL)
- PTH: (15 - 65 pg/mL)
- Alkaline phosphatase: (0 - 281 u/L)
- Calcitriol (1,25 DI-OH VIT D): (19.9-79.3 pg/mL)
Discussion
The global incidence of nutritional rickets is rising despite decades of decline, particularly in the United States1,2. Seven different children at an inner-city university hospital in New Jersey were found to have nutritional rickets over a four-year time frame. Eighty-six percent of these children were exclusively breastfed for some period of time during infancy. Breast milk is often considered the ideal form of nutrition given its well-studied benefits to an infant; however, breast milk alone does not provide an adequate amount of vitamin D to a growing infant. The amount of vitamin D in breast milk depends heavily on the vitamin D status of the mother. Mothers with darker skin have been shown to require more exposure to sunlight than mothers with lighter skin to produce equal amounts of vitamin D10. Subsequently, darker-skinned infants, such as those mentioned above, having a significantly elevated risk of developing nutritional rickets. Therefore, we recommend strict adherence to vitamin D supplementation in exclusively breast-fed infants, particularly in this population.
Of note, several patients in this case series were given orthotic bracing, in addition to treatment of the underlying nutritional deficiencies. To date, there is no strong evidence that bracing has a significant role in the treatment of children with nutritional rickets11,12. However, in these several cases, orthoses were used as an adjunct to address clinical manifestations of the disease. Additionally, alkaline phosphatase (ALP) levels were frequently recorded for these patients. While useful in differentiating between rickets and other “mimicking” diagnoses, ALP may also be elevated after acute fracture, given the increase in bone metabolism13; two patients presented with acute fractures secondary to fragility in the setting of nutritional rickets at the time the alkaline phosphatase level was collected. No current data is available on the role of ALP in a new diagnosis of nutritional rickets with acute fracture.
Additionally, a Thacher score, which is used to quantify radiologic severity of rickets on a 10-point scale, was not determined for the patients discussed in this case. Presence of fraying, irregularity of metaphyseal margin, degree of concave cupping, degree of lucency, and widening of the zone of provisional calcification in proportion to the affected growth plate are all features that are evaluated via the Thacher score14. This score was found to be reproducible between and within observers14. The regular implementation of this score can be helpful in identifying the true prevalence of nutritional rickets and osteomalacia globally, as this value remains unknown2.
Clinically, nutritional rickets can often be mistaken for Blount’s disease, osteogenesis imperfecta, skeletal dysplasia, a manifestation of renal insufficiency, or even normal variations15. When promptly recognized and treated, the prognosis of nutritional rickets is favorable. Even after several months of therapeutic replacement, as seen in these patients, there can be near complete resolution of symptoms. However, if untreated, it can result in harmful complications including pathologic fractures, permanent bone deformity, and the need for possible orthopedic surgical intervention. In the seven cases mentioned above, prompt intervention upon diagnosis likely avoided progression and possible sequalae of disease. This highligts the fact that early detection and intervention is paramount. None of the aforementioned patients required orthopedic surgery given improvement or resolution of symptoms after the prompt intervention they received.
Recommendations / Conclusion
These seven clinical vignettes illustrate that healthcare providers in the United States may not be considering nutritional rickets as part of a differential diagnosis for children presenting with orthopedic concerns. Given its perceived rarity, providers may overlook this condition and subsequently delay therapeutic dosing of calcium and vitamin D. Primary care providers and pediatricians should be made aware of the increasing prevalence of nutritional rickets; emphasizing the importance of increased clinical suspicion, particularly in infants who have been exclusively breast fed and those who have darker skin. Early intervention with therapeutic dosing of calcium and vitamin D is key and can help to avoid preventable orthopedic surgeries.
The Dietary Guidelines for Americans and the American Academy of Pediatric recommend all breastfed infants be supplemented with 400 IU/day of vitamin D16,17. This should be continued until the child has begun consuming solid foods, which is generally around 12 months of age. Adherence to daily dosing of a medication poses limitations18,19, and there is evidence that a single high dose (300,000 – 600,000 IU) vitamin D given intramuscularly is effective20-22. However, this administration poses higher risks for side effects, with lower dosing (between 150,000 - 200,000 IU) mitigating some of these adverse effects20,23. This one-time dosing may be of particular benefit for patients with lower health literacy or other difficulty navigating the healthcare system. Supplementation, in whichever form, is particularly important in infants with darker skin. The recent literature varies on recommendations for the appropriate dosing of vitamin D for children with nutritional rickets, but as of 2017, it is suggested they be treated with the following regimen of vitamin D for a minimum of 3 months6: <12 months old: 2000 IU qd, 12 months–12 years: 3000–6000 IU qd, >12 years: 6000 IU, with single high dose able to be used in resource-limited settings.
Continued vitamin D administration depends on the clinical response; some recommend lifelong supplementation given persistent underlying risk2, but others recommend discontinuation once clinical presentation and laboratory values have returned to the expected range. There is also evidence that supplementation of the mother alone was sufficient to raise serum vitamin D levels in deficient infants. Serum levels of vitamin D were significantly higher in exclusively breast-fed infants whose mothers were supplemented with vitamin D3 60,000 IU qd/10 days, when compared to unsupplemented mothers24,25. Regardless of the avenue, it is paramount these children receive adequate vitamin D dosing as soon as deficiency is detected.
In order to prevent nutritional rickets, it is recommended that physicians and public health workers promote vitamin D supplementation of mother and infant in the short term, and food fortification in the long term26,27. Additionally, it is important to both recognize and address the influence of factors such as socioeconomic status, housing, and cultural practices on the development of vitamin D deficiency and nutritional rickets2. Children and infants with darker skin who are exclusively breast fed are at the highest risk, and therefore maintaining a high clinical suspicion for this diagnosis can help to minimize easily preventable orthopedic interventions and multiple other sequalae of nutritional rickets.
Disclosures
The authors have no financial or commercial disclosures.
Ethical committee approval was not indicated. Patient consent was not obtained given the retrospective nature of the case series. All identifiable information, including personal details and dates of service, has been excluded to maintain confidentiality.
Funding
None
Study Approval
The Rutgers Institutional Review Board has approved this study. #Pro2020002886
References
- Nutritional Rickets: A Review of Disease Burden, Causes, Diagnosis, Prevention and Treatment. 2019.
- Uday S, Hogler W. Nutritional Rickets and Osteomalacia in the Twenty-first Century: Revised Concepts, Public Health, and Prevention Strategies. Curr Osteoporos Rep. 2017; 15(4): 293-302.
- Gentile C, Chiarelli F. Rickets in Children: An Update. Biomedicines. 2021; 9(7).
- Wheeler BJ, Dickson NP, Houghton LA, et al. Incidence and characteristics of vitamin D deficiency rickets in New Zealand children: a New Zealand Paediatric Surveillance Unit study. Aust N Z J Public Health. 2015; 39(4): 380-383.
- Lemoine A, Giabicani E, Lockhart V, et al. Case report of nutritional rickets in an infant following a vegan diet. Arch Pediatr. 2020; 27(4): 219-222.
- Castro S, Velasco Suarez C, Vieites A, et al. Rickets associated to the use of elemental formula: A case report. Arch Argent Pediatr. 2021; 119(1): e49-e53.
- Aung H, Soe K, Smithuis FF, et al. Case Report: Children with Severe Nutritional Rickets in the Naga Region in Northwest Myanmar, on the border with India. Am J Trop Med Hyg. 2021; 105(1): 217-221.
- Frasca D, Morganti G, Cherubini S. Nutritional rickets in twins: a case report. Pediatr Med Chir. 2013; 35(3): 130-133.
- Dubowy SM. Vitamin D deficiency rickets in a toddler. JAAPA. 2023; 36(11): 24-28.
- Quality USDoHaHSAfHRa. Vitamin D Supplementation To Prevent Rickets in Breast-Fed Babies. AHRQ Publ. 2002.
- Joshi AD, Gaur AK, Mhambre AS, et al. Effect of Lateral Single Bar Knee Orthoses in Correction of Genu Varum in Nutritional Rickets: A Randomized Trial. Indian Journal of Physical Medicine & Rehabilitation. 2018; 29(4).
- Penny JN, Sabatini CS. Rickets and Angular Bone Deformity. In: Springer International Publishing. 2020: 67-72.
- Cannalire G, Pilloni S, Esposito S, et al. Alkaline phosphatase in clinical practice in childhood: Focus on rickets. Front Endocrinol (Lausanne). 2023; 14: 1111445.
- Thacher TD, Fischer PR, Pettifor JM, et al. Radiographic scoring method for the assessment of the severity of nutritional rickets. J Trop Pediatr. 2000; 46(3): 132-139.
- BADS. Rickets. StatPearls. 2023.
- Prevention CfDCa. Vitamin D is needed to support healthy bone development. 2021.
- Tan ML, Abrams SA, Osborn DA. Vitamin D supplementation for term breastfed infants to prevent vitamin D deficiency and improve bone health. Cochrane Database Syst Rev. 2020; 12(12): CD013046.
- Grant CC, Stewart AW, Scragg R, et al. Vitamin D during pregnancy and infancy and infant serum 25-hydroxyvitamin D concentration. Pediatrics. 2014; 133(1): e143-153.
- Rodd C, Jean-Philippe S, Vanstone C, et al. Comparison of 2 vitamin D supplementation modalities in newborns: adherence and preference. Appl Physiol Nutr Metab. 2011; 36(3): 414-418.
- Cesur Y, Caksen H, Gundem A, et al. Comparison of low and high dose of vitamin D treatment in nutritional vitamin D deficiency rickets. J Pediatr Endocrinol Metab. 2003; 16(8): 1105-1109.
- Mittal H, Rai S, Shah D, et al. 300,000 IU or 600,000 IU of oral vitamin D3 for treatment of nutritional rickets: a randomized controlled trial. Indian Pediatr. 2014; 51(4): 265-272.
- Shah BR, Finberg L. Single-day therapy for nutritional vitamin D-deficiency rickets: a preferred method. J Pediatr. 1994; 125(3): 487-490.
- Emel T, Dogan DA, Erdem G, et al. Therapy strategies in vitamin D deficiency with or without rickets: efficiency of low-dose stoss therapy. J Pediatr Endocrinol Metab. 2012; 25(1-2): 107-110.
- Prasanna Naik PB, SV Madhu. Oral Supplementation of Parturient Mothers with Vitamin D and Its Effect on 25OHD Status of Exclusively Breastfed Infants at 6 Months of Age: A Double-Blind Randomized Placebo Controlled Trial. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine. 2017; 12(10): 621-628.
- Dawodu A, Salameh KM, Al-Janahi NS, et al. The Effect of High-Dose Postpartum Maternal Vitamin D Supplementation Alone Compared with Maternal Plus Infant Vitamin D Supplementation in Breastfeeding Infants in a High-Risk Population. A Randomized Controlled Trial. Nutrients. 2019; 11(7).
- Munns CF, Shaw N, Kiely M, et al. Global Consensus Recommendations on Prevention and Management of Nutritional Rickets. J Clin Endocrinol Metab. 2016; 101(2): 394-415.
- Uday S, Hogler W. Nutritional rickets & osteomalacia: A practical approach to management. Indian J Med Res. 2020; 152(4): 356-367.
