Lateral Versus Supine Traction Position for Intertrochanteric Femoral Fracture Nailing: A Meta-Analysis of Comparative Studies
Samuel Kwok1*, Naveen Nara1,2,3
1Department of Orthopaedics, Ballarat Health Services, Ballarat, Victoria, Australia
2Department of Orthopaedics, St John of God Hospital, Ballarat, Victoria, Australia
3Faculty of Medicine, Dentistry and Health Sciences, The University of Melbourne, Melbourne, Victoria, Australia
Abstract
Background: Hip fractures are a significant cause of morbidity and mortality in the elderly population. Surgical fixation using intramedullary nailing is common, with positioning options including lateral and supine on traction table. This meta-analysis aims to compare surgical and clinical outcomes between both techniques.
Method: A systematic search was performed on the Medline database for articles comparing lateral and supine traction nailing intertrochanteric femoral fractures, reporting at least one of the following: surgical set up time, total surgical time, blood loss, fluoroscopy use, tip apex distance, reduction quality, Harris hip scores or complications. Statistical analysis was performed using SAS v9.4. In addition to meta-analysis of differences in means, differences in standardised means were also analysed to account for heterogeneity between hospital protocols and surgical teams.
Results: Initial search returned 773 articles, of which four studies including 384 patients were included for final analysis. Set up time was increased in the supine traction group (random effects mean difference = 15.96 minutes, p = 0.026). Meta-analysis of random effects standardised means found increased total surgical time (mean difference = 0.8, p = 0.017), blood loss (mean difference = 1.1, p = 0.03) and fluoroscopy use (mean difference = 1.1, p = 0.0083). There were no statistically significant differences in tip apex distance, quality of reduction or Harris Hip Scores or complication rates between both groups.
Conclusion: Femoral nailing in the lateral position is not inferior to supine traction; and is one of the tools available for a surgeon to achieve successful fixation.
Introduction
Hip fractures are a significant cause of mortality and morbidity in the ageing population1. Approximately one quarter are intertrochanteric, with incidence expected to double over the next 25 years due to increased life expectancy2,3. Surgical fixation to allow early weight bearing remains the mainstay of treatment, with intramedullary nailing becoming the increasingly prevalent method of fixation2,3,4.
Options for patient positioning include supine on traction table and lateral on a radiolucent table. Supine on traction table has advantages including easier surgical access to synchronous injuries, option to perform the procedure without a surgical assistant and sustained controlled limb traction4,5,6. Use of a traction table does carry risk such as damage to the skin, perineum, neurovascular injury and compartment syndrome2,4,7.
Lateral nailing can be performed without a traction table and allows for easier entry point exposure, access for reaming and conversion to open; which may be particularly helpful in larger patients4,5,7. However, it may make anaesthesia access and lateral radiographs of the hip more difficult; and be contraindicated in setting of unstable spine injuries4,6,7. The aim of this paper is to compare differences between these two surgical techniques through meta-analysis.
Method
A systematic literature search was performed using Medline database in June 2022. Abstracts were reviewed by the primary author to assess for relevance prior to progressing to full manuscript review.
Inclusion criteria included comparative study type (randomised control trial, retrospective or prospective cohort study) comparison between supine traction and lateral decubitus cephalomedullary nailing techniques, pertrochanteric femur fracture pattern and measurement of at least one of the following outcomes: setup time, total surgical time (knife to skin till completion of procedure), fluoroscopy use, blood loss, tip apex distance (TAD), rate of acceptable versus unacceptable reduction, complication rate and Harris Hip Scores. Studies were excluded if they lacked a control supine traction table group, used novel intramedullary nailing devices or combined forms of surgical fixation (such as external fixator combined with intramedullary nailing).
Relevant results were extracted from each paper and analysed with the assistance of a professional statistician using SAS software v9.4 (SAS institute, Cary, NC). Random effects analysis was predominantly used due to small study sample sizes which may not reflect true population variance. Fixed effects results were provided for completeness. Although many study protocols were similar, differences in institutional practices may skew the value of absolute means for continuous variables (local variations in surgical technique, methods of estimating blood loss, use of different traction tables and intramedullary nails etc.), potentially obscuring statistically significant true differences between study groups despite a common direction of change. To compensate for this, we performed meta-analyses using both standardised and non-standardised means for continuous variables. Odds ratios were calculated for categorical variables.
Results
A total of 773 articles were retrieved from searches, with seventeen excluded due to duplication. Thirteen articles were shortlisted for full manuscript review. Seven articles were removed due to lack of control group. One article was excluded as it focused on femoral shaft rather than intertrochanteric fracture pattern. One additional study (Souza et al. 2016)3 was excluded as it reported TAD in an atypical categorical fashion (acceptable versus unacceptable) in contrast to other papers which reported a quantifiable distance. Four papers remained for final analysis, with summary of these available in Figure 1 and Table 1.
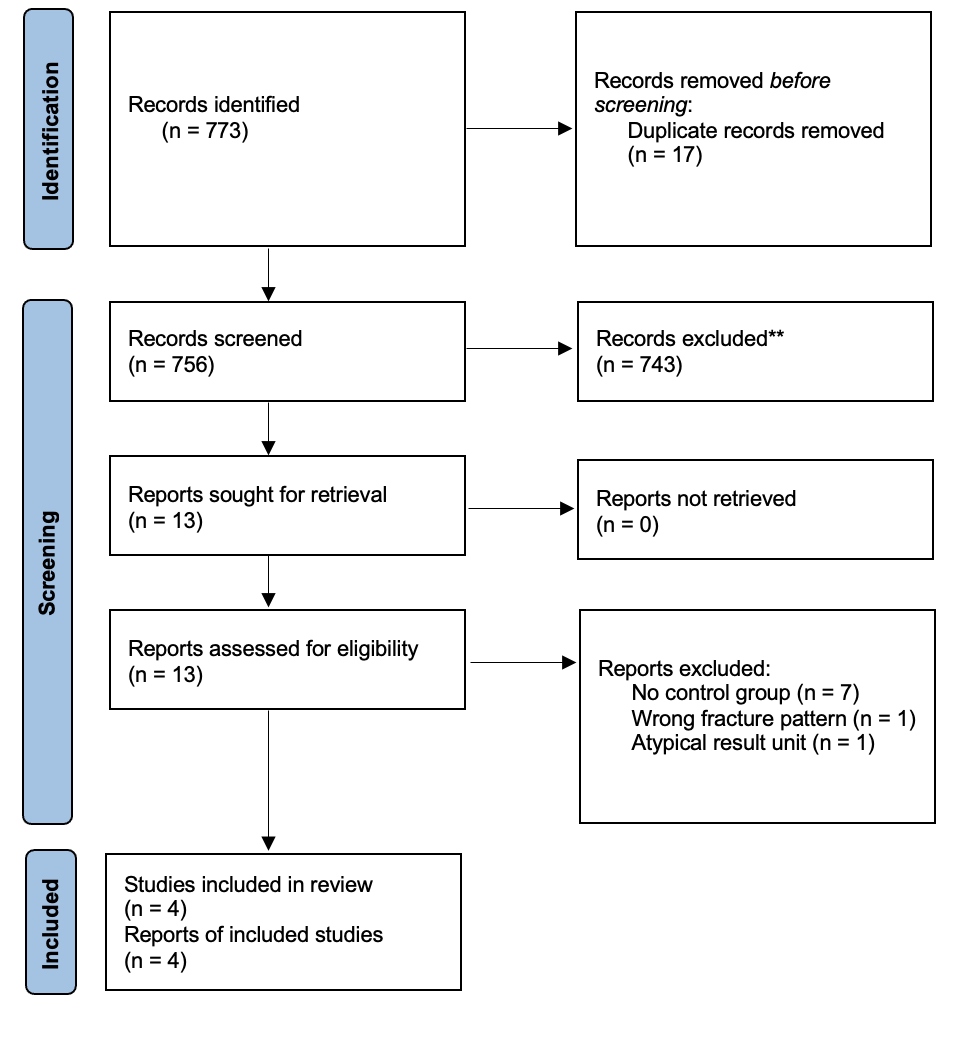
Figure 1: Prisma Diagram
Table 1: Summary of Articles
|
Authors |
Study Type |
Study Period |
Nail |
Lateral n |
Supine n |
Inclusion Criteria |
Exclusion Criteria |
|
Dogan, Erturk, Gulabi (2022)2 |
Randomised Control Trial |
Apr 18'- Apr 19' |
TST Medical Proximal Femoral Nail |
40 |
40 |
Age > 60 |
Multiple fractures |
|
Li et al. (2020)8 |
Retrospective Cohort Study |
Jan 13' - Apr 18' |
Synthes PFNA |
52 |
50 |
Age > 60 |
Not suitable for intramedullary nailing |
|
Sonmez et al. (2017)4 |
Randomised Control Trial |
2011 - 13' |
Synthes PFNA |
42 |
40 |
Unstable intertrochanteric fracture |
Use of general anaesthetic |
|
Xue et al. (2013)10 |
Randomised Control Trial |
May 09' - Aug 10' |
Synthes PFNA |
60 |
60 |
Age ≥ 60 |
Multiple fractures |
# Altered mental state, acute or chronic infection, severe cardiac, hepatic or renal comorbidities, concurrent chemo or hormonal therapy, pregnancy, participation in other clinical trials within 6 months.
PFNA = Proximal Femur Nail Antirotation
Demographics
A total of 384 patients were included over four studies, with 194 undergoing lateral nailing and 190 undergoing supine traction nailing. Mean age was reported in all four studies and was similar in both groups (lateral group 77.2 years versus supine traction group 76.3 years). Three studies reported patient sex, with split between both groups being similar (lateral group 47.4% male versus supine traction group 46.7% male).
Intraoperative Outcomes
Surgical set up time was reported in three studies. Two studies found the supine traction table group had a statistically significant longer set up time (Dogan et al. 2022, Li et al. 2020)2,8. With both random and fixed effects analysis, as well as mean and standardised mean analysis, there was a statistically significant increased setup time with use of a traction table (random effects mean difference = 15.96 minutes, 95% confidence interval (CI) 4.77 – 27.15 minutes, p = 0.026) [Figure 2].
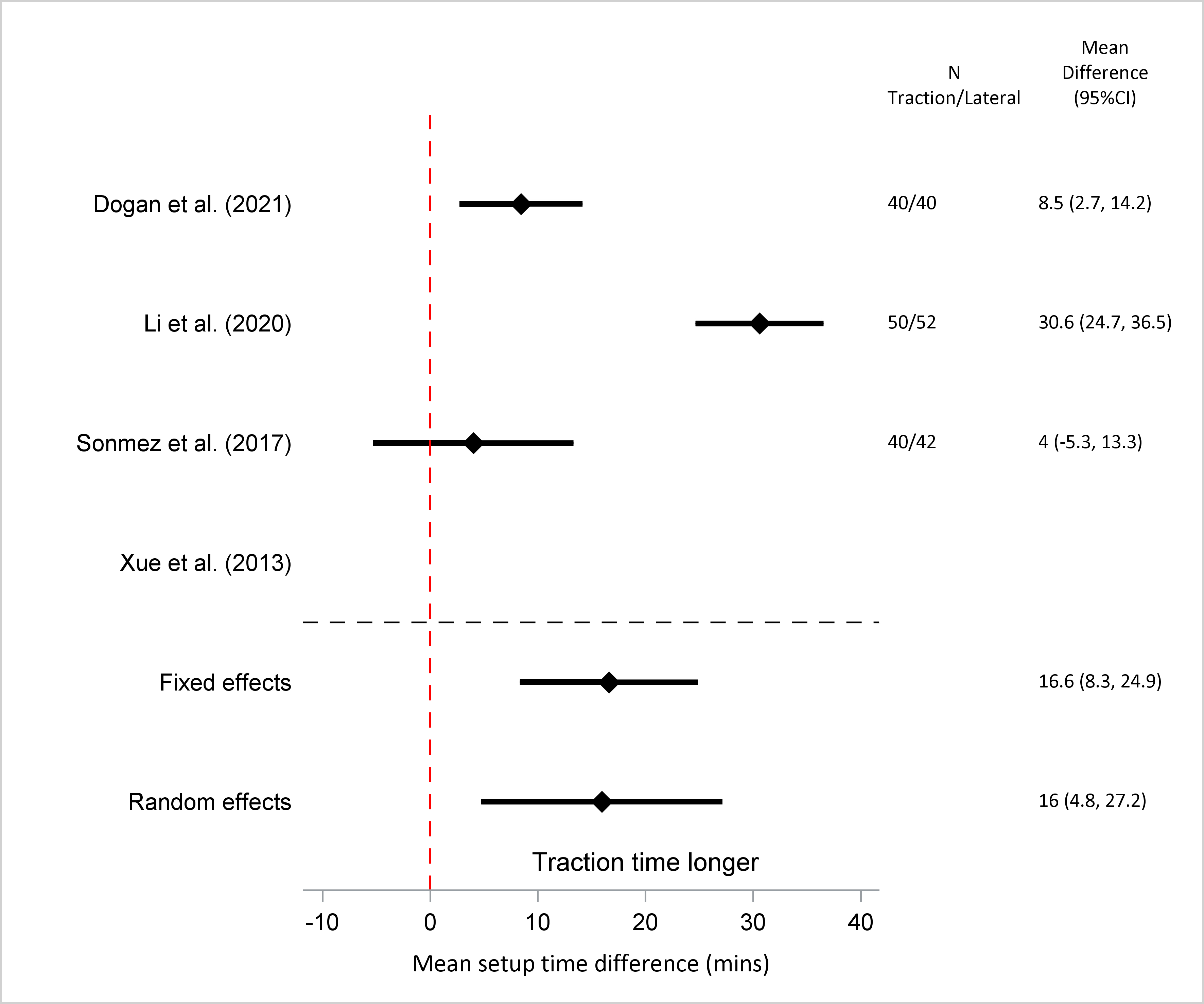
Figure 2: Setup Time (mean difference)
Mean total surgical time was recorded in four studies, with three out of four finding a longer but not statistically significant difference in total surgical time in the supine traction group. Random effects meta-analysis found an increased mean total surgical time in the supine traction group but the difference was not statistically significant (random effects mean difference = 6.4 minutes, 95% CI -15.8 to 28.5 minutes, p = 0.43). However, a statistically significant longer total surgical time for supine traction nailing was found with meta-analysis of standardised means (random effects standardised mean difference = 0.8, 95% CI 0.3 – 1.3, p = 0.017) [Figure 3].
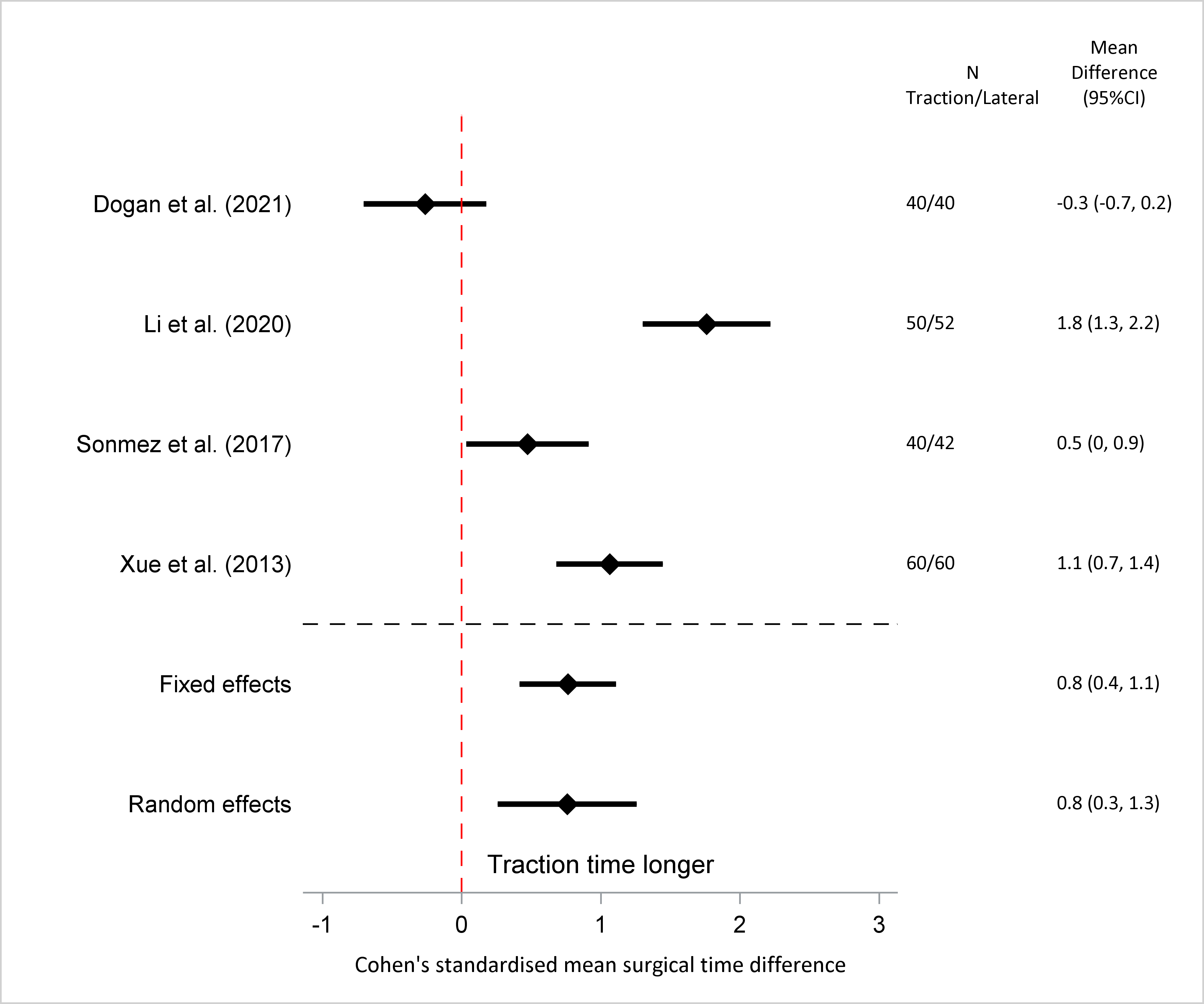
Figure 3: Total Surgical Time (standardised mean difference)
Blood loss was recorded in three studies, with Li et al. 20208 finding a significantly increased loss in the supine traction group. Pooled mean blood loss results between both groups were not found to be statistically significant (random effects mean difference = 28.9ml, 95% CI -103.3 to 161.0 ml, p = 0.45), however a significant increase was found in the supine traction group with standardised mean meta-analysis (random effects standardised mean difference = 1.1, 95% CI 0.3 – 1.9, p = 0.03) [Figure 4].
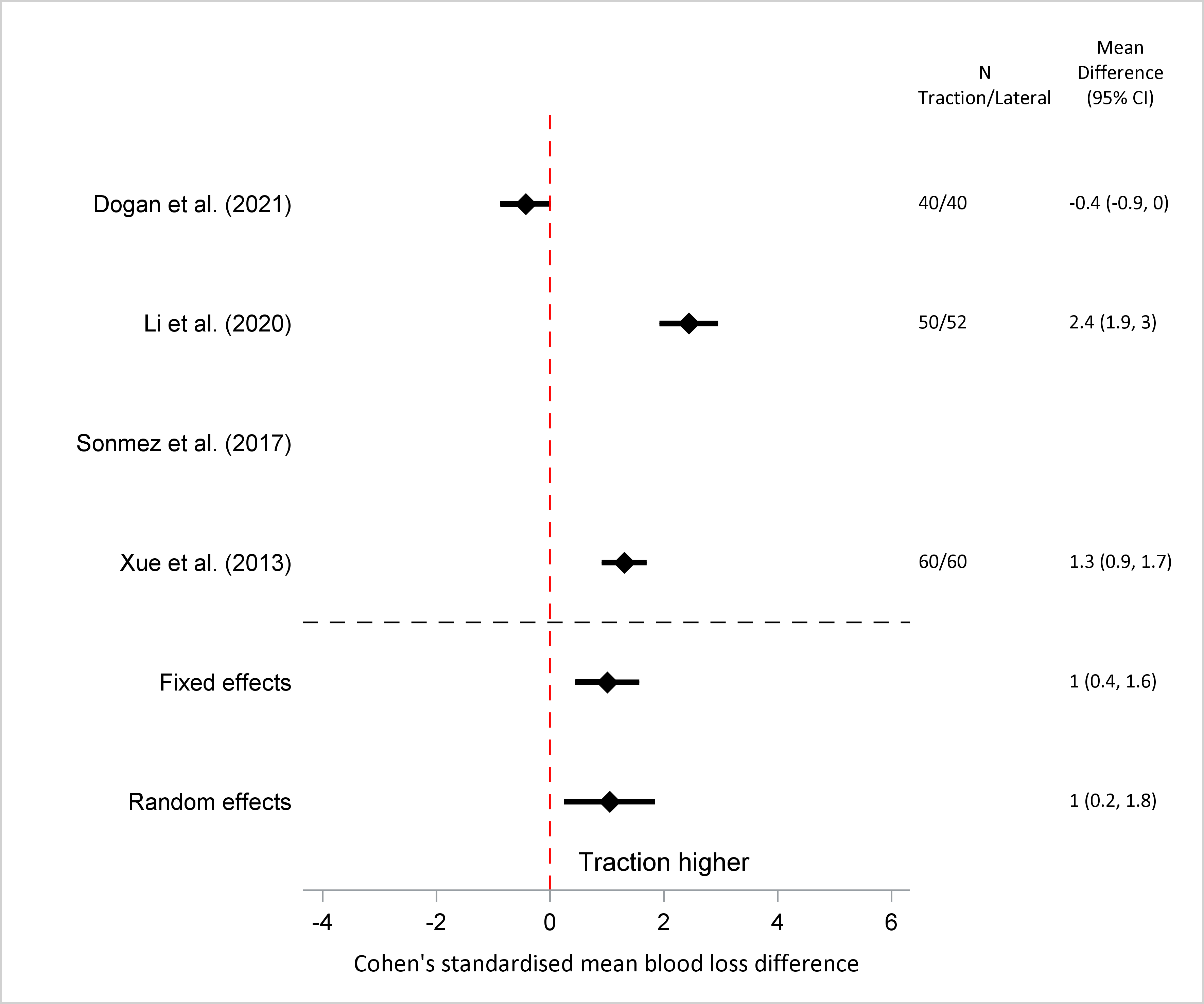
Figure 4: Blood Loss (standardised mean difference)
Fluoroscopy use was recorded in all four studies however two studies recorded use in time while the remaining two used number of shots. As fluoroscopy time is highly linked to number of shots taken, standardised mean analysis was used to combine the results from all four studies. A statistically significant increased use of fluoroscopy was found in the supine traction group (random effects standardised mean difference = 1.1, 95% CI 0.6 – 1.6, p = 0.0083) [Figure 5].
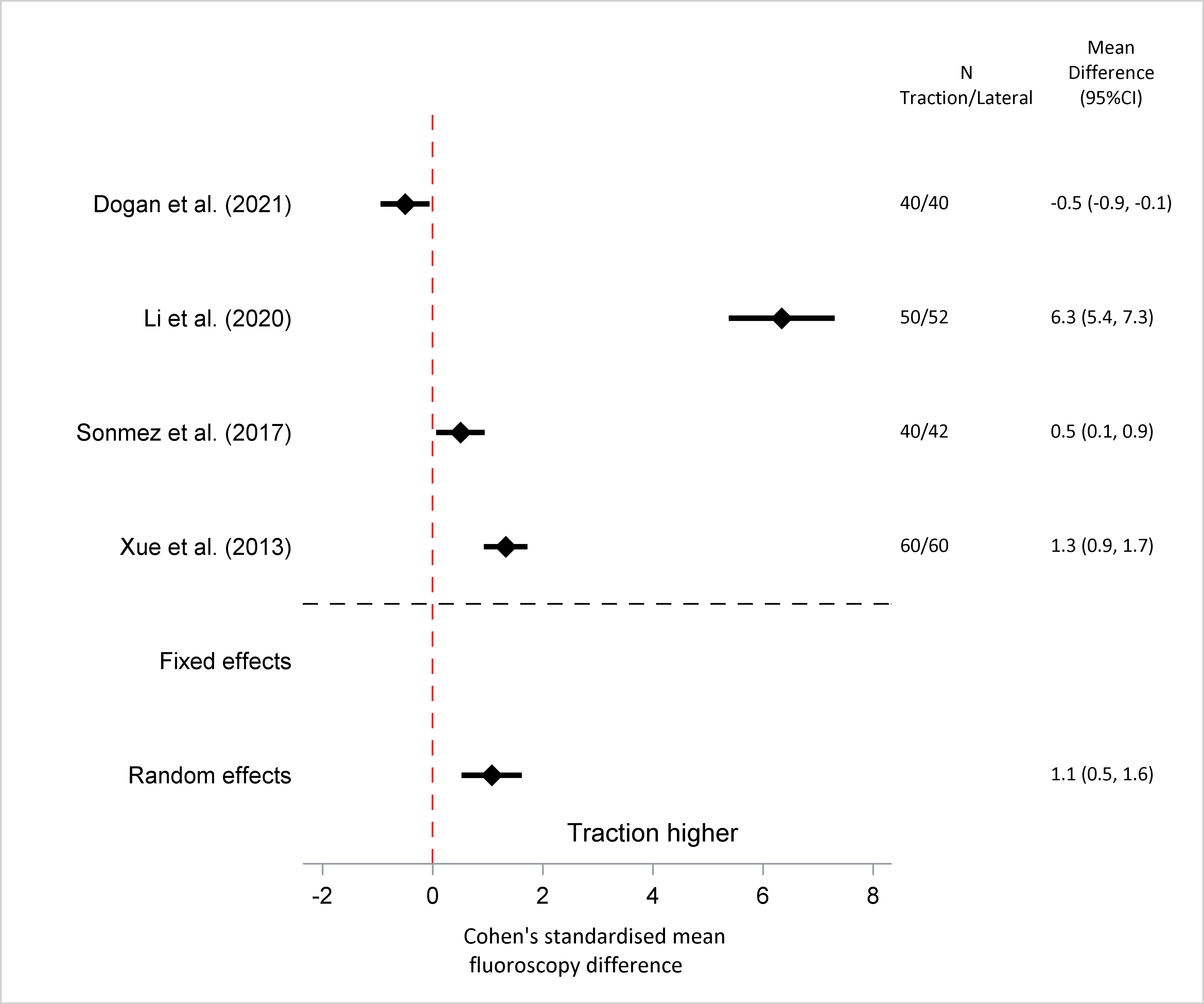
Figure 5: Fluoroscopy Use (standardised mean difference)
Postoperative Outcomes
TAD was measured in two studies, with neither finding a significant difference between each group. Pooled meta-analysis did not show a statistically significant difference between means or standardised means (random effects mean difference = 0.5mm, 95% CI -108.9 to 109.8, p = 0.96).
Quality of reduction was measured in two studies using modified Baumgartner criteria, with neither finding a significant difference between both groups. Overall total rate of unacceptable reductions was low, with 5.19% in the lateral and 2.63% in the supine traction groups. Pooled meta-analysis of odds ratios found no statistically significant difference in reduction quality (random effects odds ratio 1.48, p = 0.86).
Harris hip scores were reported in three studies, two after a minimum of one year and one after a minimum of twelve weeks. No study in isolation, nor with pooled meta-analysis of mean scores or standardised means found a statistically significant difference between both groups (random effects mean difference = 0, 95% CI -47.6 to 47.5, p = 0.998).
Complications were reported in two studies, with a total of four patients in the lateral group (3.6%) and five patients in the supine group (4.5%).
Discussion
Lateral position is one of the many tools available to assist a surgeon during femoral nailing. The purpose of this article is not to advocate superiority of one technique over the other, but to instead highlight lateral nailing as a viable alternative.
One of the significant benefits of lateral nailing is that it does not require a traction table. This can be particularly useful when a traction table is not available or is unexpectantly found to be broken; as in the experience of our senior author which inspired this paper. Given the increased labour and expertise required to set up a traction table, it is not surprising longer set up times were found in this group8. Although time savings may not be long over a single case, time savings can often compound over the course of a whole operating list.
Although some authors have raised concerns that lateral nailing may be more technically challenging, particularly when obtaining x-rays, there were no statistically significant differences in total surgical time2,9. Unexpectedly, standardised mean analysis found total surgical time may be lower in the lateral group, however the magnitude of saved time is not known. The difficulty of imaging the hip in lateral position may be offset by other benefits such as easier instrumentation, easier conversion to open and ability to apply reduction manoeuvres in all axes4,10. This difference may be worth investigating further in future studies given prolonged surgical time in the elderly may increase mortality4.
Despite the difficulties of lateral position imaging, the difference of standardised means found a statistically significant lower use of fluoroscopy in the lateral group2,9. The most commonly described technique for visualising the lateral hip x-ray is by rotating the image intensifier over the table by ten to twenty degrees, accounting for femoral anteversion to show a view in line with the femoral neck6,7. Possible explanations of this finding include a surgical or radiology team more familiar with lateral nailing technique (resulting in more efficient fluoroscopy use), or easier reduction and entry point establishment in the lateral position requiring less shots to be taken during instrumentation. Standardised mean blood loss was higher in the supine traction table group, which could coincide with the longer operative times. However, this difference was extremely small (pooled mean difference of thirty millilitres, with no individual study findings a difference higher than fifty millilitres) and unlikely to be of clinical significance.
The quality of fracture reduction in both groups were similar. There were no differences in the rate of unacceptable reduction based on modified Baumgartner criteria between both groups, with rates lower in both groups than those found in recent literature11. No statistically significant difference was found between the mean TAD of both groups. However, it is noteworthy that both studies reporting TAD (DoÄan et al. 2022 and Sonmez et al. 2017) had a lateral group with a mean distance slightly above 25mm: the conventional upper limit of safe TAD before increased risk of lag screw cut out12. DoÄan et al. 20222 in particular had a wide confidence interval, almost double the spread of their supine traction control group. Unfortunately, complications were not reported in these two studies so it cannot be determined if cut out or other complications occurred more frequently in either group. This may suggest although good fracture reduction can be achieved in the lateral position, visualising the tip of the screw during instrumentation may be difficult and particular care should be exercised to achieve an optimal tip apex distance.
Overall final clinical outcomes between both groups seemed similar, with no difference in Harris Hip Scores or complication rates between both groups. Four patients in the lateral group had complications (one superficial infection, one deep vein thrombosis and two patients with persistent hip pain), compared to five in the supine traction group (two patients with persistent hip pain, one with wound fat necrosis, one deep wound infection, one deep vein thrombosis), with surgical position unlikely to affect these outcomes.
There are areas in our study which could be improved in future research. Although femoral nailing is a common orthopaedic procedure, significant heterogeneity would exist from local protocols and preferences. More detailed descriptions and standardised surgical methods would help produce more comparable results. Despite lateral positioning being advantageous in obese patients, only one of our articles recorded body mass index, a potential source of bias if patients were not evenly distributed between both study groups5,6. Common outcomes, such as amount of fluoroscopy use and reduction quality, should be reported with standardised units to allow easier comparison between studies. In addition, given the potentially high TAD in the lateral group, more research is necessary to determine if nailing using the lateral position is associated with a higher risk of nail cut out.
Conclusion
Femoral nailing is a common treatment of pertrochanteric femur fractures. Both surgical techniques produce similar outcomes with no significant differences in quality of reduction, complications and Harris Hip Scores. Set up time is slightly faster in the lateral group likely owing to less labour required. Lateral nailing may have less bleeding, fluoroscopy use and shorter procedure time however the size of these differences is unknown. Finally, given the potentially higher TAD in the lateral group, special care should be exercised to ensure acceptable TAD is achieved when nailing in this position.
Disclosure Statement
No authors have conflicts of interest to declare.
References
- de Oliveira JN, Hungria JO, Bellan DG, et al. Lateral decubitus for treating pertrochanteric fractures using cephalomedullary nails. Rev Bras Ortop. 2015; 50(4): 409-15.
- Dogan N, Ertürk C, Gülabi D. Is proximal femoral nailing of unstable intertrochanteric fractures in the lateral decubitus position without a traction table as safe and effective as on a traction table? Injury. 2022; 53(2): 555-60.
- Souza EF, Hungria JO, Rezende LR, et al. Comparative study between lateral decubitus and traction table for treatment of pertrochanteric fractures with cephalomedullary nails. Rev Bras Ortop. 2016; 52(1): 24-28.
- Sonmez MM, Camur S, Erturer E, et al. Strategies for Proximal Femoral Nailing of Unstable Intertrochanteric Fractures: Lateral Decubitus Position or Traction Table. J Am Acad Orthop Surg. 2017; 25(3): e37-e44.
- Sloan M, von Keudell A, Walley KC, et al. Closed Cephalomedullary Nailing with Patient in Lateral Decubitus Position for Repair of Peritrochanteric Femoral Fracture. JBJS Essent Surg Tech. 2016; 6(1): e6.
- Carr JB, Williams D, Richards M. Lateral decubitus positioning for intramedullary nailing of the femur without the use of a fracture table. Orthopedics. 2009.
- Bishop JA, Rodriguez EK. Closed intramedullary nailing of the femur in the lateral decubitus position. J Trauma. 2010; 68(1): 231-5.
- Li M, Chen J, Ma Y, et al. [Comparison of proximal femoral nail anti-rotation operation in traction bed supine position and non-traction bed lateral position in treatment of intertrochanteric fracture of femur]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2020; 34(1): 32-36.
- Liu HT, Wang IC, Yu CM, et al. Closed femoral nailing in lateral decubitus position without a fracture table: a preliminary report of fifteen patients. Chang Gung Med J. 2005; 28(9): 629-35.
- Xue L, Zha L, Chen Q, et al. Randomized controlled trials of proximal femoral nail antirotation in lateral decubitus and supine position on treatment of intertrochanteric fractures. Scientific World Journal. 2013; 2013: 276015.
- Bhaskara K, Taranath N. Prospective study of effect of quality of reduction of intertrochanteric fractures on functional outcome. National Journal of Clinical Orthopaedics. 2019; 3(2): 88-91.
- John B, Sharma A, Mahajan A, et al. Tip-apex distance and other predictors of outcome in cephalomedullary nailing of unstable trochanteric fractures. J Clin Orthop Trauma. 2019; 10(Suppl 1): S88-S94.
