Hip Arthroplasty in Young Patients: Analysis of the New Zealand Joint Registry
Sean T. Gerlach*, Dillon J. MacIntyre, Tim P. Gregg
Wellington Regional Hospital, Wellington, New Zealand
Abstract
Purpose: The aim of this study was to look into the New Zealand Joint Registry (NZJR) data on total hip arthroplasty (THA) in paediatric and adolescent patients aged 20 and under. Specifically, indications for THA, trends in implants and outcome data.
Methods: An analysis of all patients aged 20 and under, recorded in the NZJR from December 1999 until January 2021. Review of similar international reports and NZ adult data undertaken.
Results: We identified 115 THA performed in patients aged 20 and under in the NZJR. Mean age at primary surgery is 17.9 years. Indications included avascular necrosis (24%), fracture (6%), tumour (3.5%), inflammatory conditions (16.4%), post-infective (6.1%), SUFE (8.7%) and various other disorders. A total of 9/115 THA were reported as being revised in the study period with a revision rate per 100 component years of 0.69. Bearing surface has trended towards ceramic heads. Cementless implants have been the most commonly utilized. The approach is almost exclusively posterior (79%). Head size has increased from formerly being 28 or less to now 32 and above.
Conclusions: Rates of THA in this population remain very low, in keeping with international data. Indications are similar to those seen in other registry studies. Trends mimic those seen internationally and in adult cohorts with cementless implants and larger ceramic heads being favored. Revisions were recorded in 9/115 patients with polywear being the most common indication. Outcome measures were excellent with a mean Oxford hip score of 37.4 at 6 months post operatively.
Introduction
Hip arthroplasty has long been an appealing solution to end-stage hip degenerative disease.
Over the years, implants and techniques have improved, with a trend in international registry data being towards longer implant survivability1. In children and adolescents, a variety of pathologies can lead to end-stage hip disease and the role of hip arthroplasty has been considered for some time2. However, hip pathology in children and young adults varies considerably from that of older adults. While osteoarthritis is responsible for nearly 90% of primary total hip arthroplasties in the adult population in NZ, in young patients by contrast, conditions such as severe juvenile inflammatory arthritis, developmental dysplasia, various forms of osteonecrosis and tumours are the more common underlying diagnoses leading to hip arthroplasty3,4. These conditions often bring unique anatomic considerations meaning surgery is more complex and extensive5. In addition, the life expectancy and activity level of younger patients means it is expected that patients will outlive their prosthesis necessitating future revision surgery6. As repeated revision procedures are associated with increasingly less satisfactory outcomes, it is imperative that the aim of the first procedure be to obtain the best outcome possible in the clinical circumstance7. Successful THA in this population requires host optimization, comprehensive preoperative planning, and appreciation of underlying disease-specific deformity to yield optimal results.
Previous registry and cohort studies from overseas looking into paediatric hip arthroplasty have reported on various aspects of indication, implant selection, implant survival, revision rates and complication8-11. The NZJR has yet to be studied in this way despite the New Zealand population, in particular Maori and Pacific Islanders, having some of the highest rates of paediatric hip conditions, particularly SUFE, in the world12.
The aim of this study was to analyse the data for paediatric THA in New Zealand, specifically: indication, trends in bearings and cementing and revision with comparisons to that of the international data and NZ adult population.
Methods
This was a retrospective observational study based on data from the NZJR. We identified all patients 20 years or younger (n = 115) reported to have primary hip joint replacement during the period January 1st 1999 to December 31st 2022. No exclusion criteria were applied. All data available from the registry was analyzed. This included demographics: age at the time of surgery, sex, and ethnicity. It also included indications for surgery, though the detail was variable. Surgical factors such as approach, implants, bearing surface, cementing and finally outcome and revision data. No cases were excluded even if some values were missing. Indications were grouped into eight categories. Specific patient data such as details of underlying diagnosis, severity and previous surgery were not available in the registry data. Registry data as provided from the NZJR was split into 1999-2007 as bulk data and yearly thereafter.
Statistics
Rate/100 component years
Revision outcomes were provided in the form of rate/100 component years, equivalent to the yearly revision rate. It is derived by dividing the number of prostheses revised by the observed component years multiplied by 100.
Results
Demographics
A total of 115 primary THA for patients 20 and under have been performed in New Zealand since the inception of the national registry 23 years ago. This makes up 0.00068% of the total 167,670 THA performed in that period. Numbers of THA have seen a surge in the last 3 years of the period studied, with a dip again in 2020 (Covid-19 lockdown restrictions).
The mean age for this cohort was 17.9 (range 13-20). BMI was recorded for 39 of the 115 cases, with an average of 26.8 (range 18-43). The sex of patients was 47% female and 53% male. Maori made up 17.4% of the cohort. (Table 1)
Table 1: Patient demographics
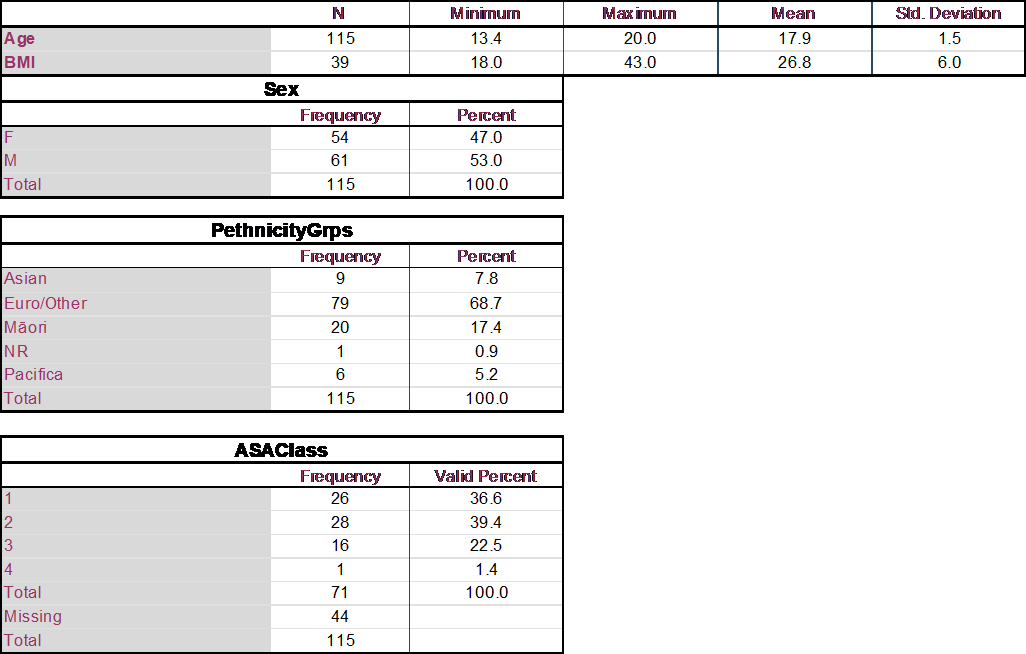
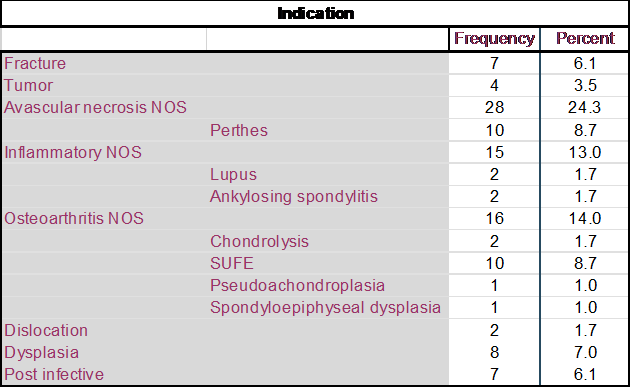
Indication
Data on the specific indications for surgery was limited due to a lack of access to patient records. Recorded data was broad but included fracture at 6%, tumour at 3.5%, avascular necrosis at 33%, systemic inflammatory conditions at 16.5%, osteoarthritis at 26% and post-infective at 6%. (Table 2)
Table 2: Indication for surgery
Surgical data
Approach data was reported for 104/115 patients and revealed a majority posterior 82/104 (78.8%), followed by lateral 16/104 (15.4%), only 5/104 anterior (4.8%) and one patient receiving a trochanteric osteotomy.
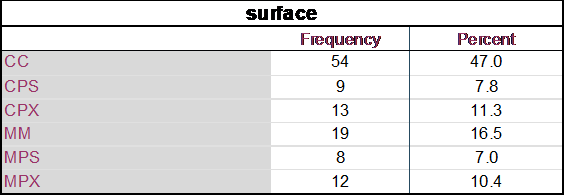
Head size, 36.5% were size 28, 25.2% size 36 and 23.5% were size 32 (full list Table 3).
Cement on cement for 1/115, uncemented the majority 89/115 (77.4%) and hybrid 25/115 (22%) (Table 4).
Surfacing (Table 5) was majority ceramic on ceramic or ceramic on polyethylene.
Table 3: Head size
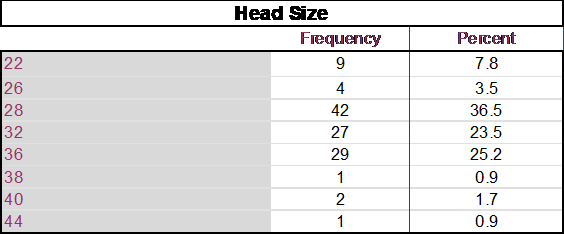
Table 4: Cementing
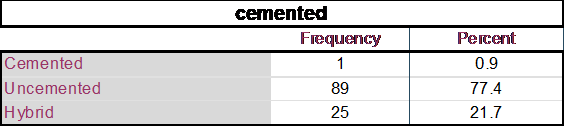
Table 5: Surfacing
Trends
Several trends were observed in the data. Pre-2008 head size was majority 28 (83%), subsequently the trend has been towards larger head size (Figure 1).
Approach meanwhile has been consistently posterior over time.
Cementless implants made up 66% of cases pre-2008 but since then have made up 87%. Hybrid has made up the remainder, with only one cement-on-cement implant being placed in the registry.
Surfacing of metal on metal made up 35% of bearings pre-2008, while ceramic on ceramic only 19%. Pre-2008 metal heads made up 62% of implants and ceramic 38%. Since 2008, 44/62 have been ceramic on ceramic (71%). Overall ceramic heads have been placed in 90% of cases since 2008 (Figure 2).
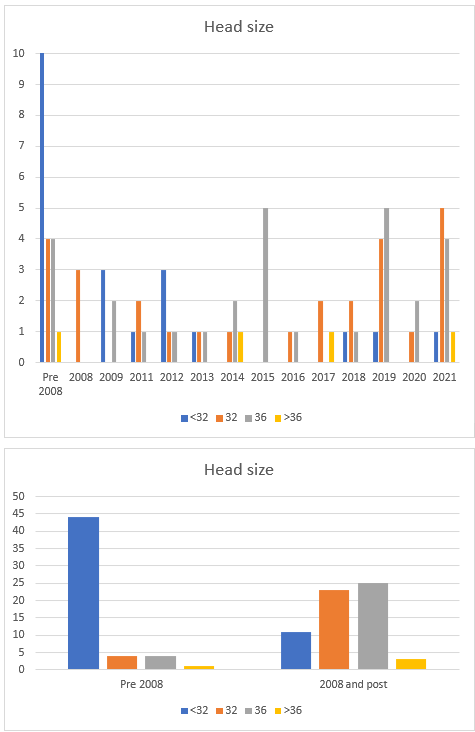
Figure 1: Trends in head size.
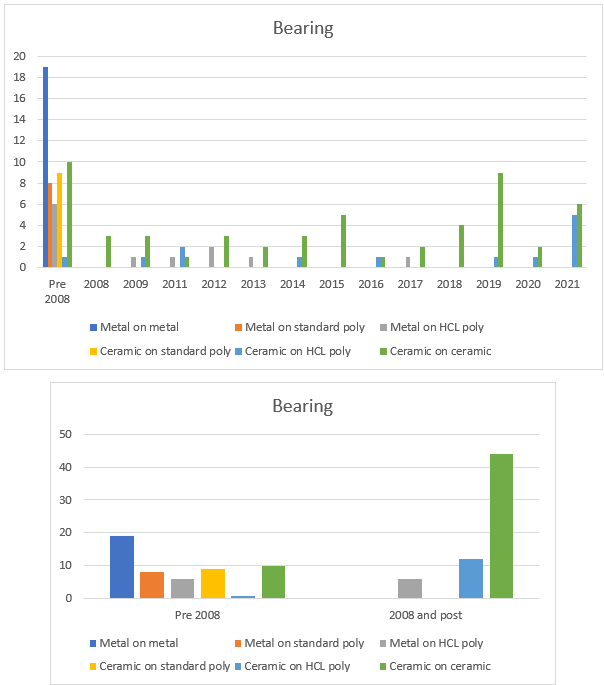
Figure 2: Trends in bearing surface.
Outcomes
Oxford scores at 6 months were only available for 14/115 patients (12%). Of these, 50% reported scores >42 and 4/14 reported scores 34-41. The overall mean Oxford hip score was 37.4. A total of 9 revisions were reported for this cohort, 6 in female patients, and 3 in male. The rate per 100 component years was 0.69 (0.32-1.32 95% CI). Time to revision was an average of 13.84 years (range 6.11-18.36). Indications for revision are outlined in Table 6.
Table 6: Revisions
|
|
Year Primary |
Age |
Time to Revision |
Reasons |
|
1 |
1998 |
19.2 |
15.87 |
Impingement back of neck |
|
2 |
1999 |
18.1 |
16.05 |
Polyethylene wear |
|
3 |
1999 |
18.1 |
16.05 |
Polyethylene wear |
|
4 |
2004 |
19.1 |
6.11 |
LooseningFem |
|
5 |
2001 |
19.7 |
18.36 |
Osteolysis |
|
6 |
2002 |
17.4 |
10.41 |
Polyethylene wear |
|
7 |
2003 |
15.5 |
15.09 |
Polyethylene wear |
|
8 |
2003 |
15.4 |
15.55 |
Polyethylene wear |
|
9 |
2008 |
18.7 |
11.10 |
LooseningAcetab |
Discussion
This registry-based cohort study is the first analysis of the NZJR data for hip replacement in young patients. It has included 115 patients in total, aged 20 or younger, recorded in the registry.
Proportion of registry
Overall, hip replacements for patients aged 20 or younger in NZ make up less than 0.001% of the registry, which is lower than the findings of other registry-based studies13. An Australian registry study of 297 primary THAs performed in patients younger than twenty-one years of age representing 0.08% of all THA procedures reported during the period studied. In their cohort, osteonecrosis (29% of procedures) and osteoarthritis (28%) were the most common diagnoses. However, 12% had various types of dysplasia and 15% had autoimmune arthritis reported as the primary diagnosis. An additional 9% involved treatment for a bone tumour8.
The NZ numbers seem low when considering NZ has some of the highest rates of paediatric hip conditions, particularly SUFE, in the developed world. In a previous NZ registry study performed for the period of 1999 to 2008, Boyle et al. identified 117 patients with SUFE who had undergone THJR, however, the mean age at the time of operation was 48.514. Developmental dysplasia/congenital dislocation cases number 3,322 in the NZ registry to date. As these patients clearly do not have early THA, this likely indicates the success of hip preservation techniques at younger ages. But also raises the question of whether approaches such as arthrodesis are favored by paediatric surgeons for this younger age group with severe disease15. In a 2016 survey of members of the Paediatric Orthopaedic Society of North America and the American Association of Hip and Knee Surgeons, the preference for treatment for end-stage unilateral hip arthritis in 18-year-olds found that surgeons who believed that revision of THA later in life posed a significant problem were more likely to recommend arthrodesis while those who valued function as a young adult leaned toward THA16. Contemporary improvements in hip implants, as well as fellowship training in joint arthroplasty, appeared to create bias toward total hip arthroplasty in young patients16.
The relatively low number of tumour prostheses raises the question of underreporting of these cases, particularly of custom megaprostheses. In a 2022 review of the UK National Joint Registry, clear disparities between NJR data and other published literature suggest a significant degree of underreporting of megaprosthesis cases to the NJR17.
It is noted that in the years 2019 and 2021 there was a near doubling of THA performed in this population and raises the question of whether this is a new trend, however, observation over the coming years is needed (Figure 3, 4).
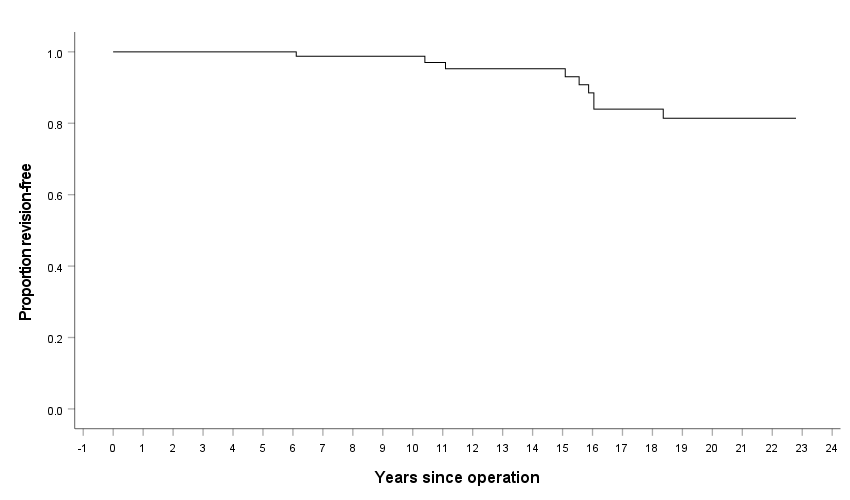
Figure 3: Kaplan-Meier survivability graph.
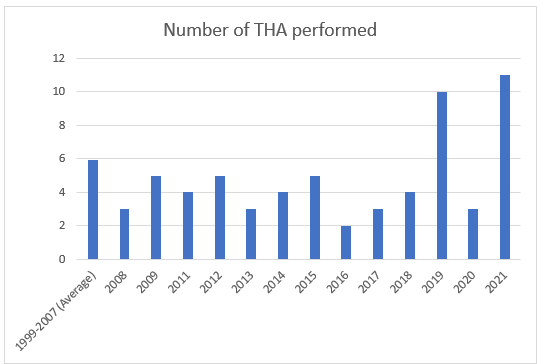
Figure 4: Number of THA performed.
Trends in THA
Trends of THA in young patients over the years have resembled those of the adult population. This data set has shown a trend toward larger ceramic heads, uncemented implants and surfacing of ceramic on ceramic or ceramic on HCLP.
NZJR adult data also shows a trend towards more hybrid and cementless implants with cemented implants now making up only 5% in 20214. While there is a steadily reducing number of ceramic-on-ceramic bearings in adults since 2010, there has been a significant increase in ceramic on HCLP4. This trend cannot be seen to match that of the paediatric group in this study. Head size follows similar trends in adult data with <=32 now making up only 10% compared to over 80% pre-20084. This trend can be attributed to the use of HCLP which has improved wear characteristic making larger head sizes more feasible and thereby reducing dislocation risk.
International registry data from Australia for the period 1999-2012 was analysed by Sedrakyan et al. They found cementless fixation was used in 69% of procedures, and hybrid fixation involving cementation of only the femoral component was used in 21%. The most common bearing surface was ceramic-on-ceramic (40%), followed by metal-on-cross-linked polyethylene and metal-on-metal (22% each). Ceramic-on-XLPE bearings were less common (8%), and metal-on-conventional polyethylene was used in 4%. This study unfortunately did not analyse the trends over time, however8.
An Oxford review of the UK NJR in 2018 by Metcalfe et al. analysed 2003 to 2017 looking at trends in patients aged 20 and under. Similar to our NZ data they found a trend to more CoC and CoP with CoC being the dominant bearing since 20059.
The posterior approach has been consistent across time. In this data set 79% underwent a posterior approach while in the NZJR overall, a posterior approach made up 68% in the same period.
Revision data
Revision data on this patient cohort demonstrated a rate of revision per 100 component years of 0.69 (95% CI 0.32-1.32). Comparison to full NZJR dataset shows similar numbers, with overall rates per 100 component years of 0.6476 (0.63-0.66)4.
When comparing this study with the available international data, revision numbers appear much lower. Based on the Kaplan-Meier analysis 100% of this cohort was revision free at 5 years, by 10 years only one revision had taken place for aseptic loosening leaving 93% revision free. Majority of revisions appear to have occurred around the 15-20 year mark secondary to polyethylene wear and all of these implants were standard poly placed pre-2004. An Australian registry study of 297 primary THAs in patients under 21 demonstrated a 5-year revision rate of 4.5% with 1 in 3 being caused by loosening or osteolysis8. A NORDIC study from 1995-2016 of patients 21 years or younger showed implant survival of 94% at 5 years, 86% at ten years and 76% at 15 years10. In a UK registry study of patients <30, the survival rate was 97.9% at 5 years, 71% at 10 years but then a significant drop and only 52.4% at 15 years11. In a French registry study of 113 hips 20 and younger a total of 17 hips were revised, with a revision-free rate at 10 years estimated at 90.3% (95% CI, 82.4%–98.9%) and a median time to revision of 21.7 years20. This study however was purely ceramic on ceramic bearings.
Longer term data is clearly needed to better establish the revision outcomes in this population, particularly given the increasing numbers of ceramic on ceramic and ceramic on HCLP.
An observation in the available data is a lack of dislocation as indication for revision. In the general NZJR population, dislocation was listed as indication for revision surgery in 37.8% of revisions pre-2008 and between 15-25% thereafter4. Similarly, in the Sedrakyan et al. analysis of the Australian joint registry of 297 THA in young patients (under age 20) found dislocation as a cause for revision in 18% of cases8. It is unclear why dislocation does not appear as a feature in this data set.
Outcome data
The NZJR randomly selects 20% of patients receiving THA annually to complete a 6 month Oxford Hip score (OHS). Of the 115 patients in this study, 14 had 6 month post operative OHS (12%). Results were very encouraging, with a high mean score of 37.4 and 78% of scores 34 and above. Similarly, OHS for the general NZJR population as of July 2021 had an average score of 40.36 (based on 36,598 THA responses) with 84% have scores 34 and above4. Findings from other paediatric THA studies echo these encouraging results. In 2020, 118 primary THA that had been performed in Sheffield, UK, had an average 5 year OHS of 37.511. While the modern day validity of the OHS has been explored by some authors19, and its use has not been verified in the paediatric population it remains the only tool available to this data set for measuring functional outcomes.
Limitations
There were several limitations to this study. In terms of data entry, patient diagnosis is entered into the NZJR records by the operating surgeon only and is not validated; this may result in inaccurate diagnosis for certain patients and consequent information bias. Another limitation is that the NZJR records only the diagnosis and not the severity disease. There were also multiple other data shortages, including pre and post-op hip scores etc. Post operative NZJR follow up with oxford hip scores are only sent out to a small random number of patients each year, thereby limiting the availability of such results within the confines of registry provided data. More detailed analysis of outcomes and complications would require access to hospital and patient data which was outside the scope of this paper.
Further research into the population group should make efforts to contact patients directly for more accurate outcome data and also access patient records for better data on indications for surgery or previous surgical interventions.
Conclusion
This is the first study looking at THA in the NZJR for patients aged 20 and younger. Over the 21 years of data collection there have been 115 recorded THR performed for this young population. While data was variable, there have been several trends apparent and comparative to those of the adult and international data. There appears to be a rising number of THA being performed in this age group but further observation is required. Nevertheless, THA in this age range makes up only a very small proportion of the NZJR despite high rates of paediatric hip conditions in New Zealand. This raises the question of whether hip salvage procedures or arthrodesis are favored by paediatric surgeons. The data demonstrated a trend towards cementless implants, larger head sizes and ceramic bearings. Outcome and revision data was very positive, with a rate of revision per 100 component years of 0.69 and mean OHS of 37.4.
Acknowledgement
Funding provided by the Wellington Surgical Research Trust.
Data access was provided by the New Zealand Joint Registry.
Conflict of Interest
The authors have no conflicts of interest.
References
- Evans JT, Evans JP, Walker RW, et al. How long does a hip replacement last? A systematic review and meta-analysis of case series and National Registry reports with more than 15 years of follow-up. The Lancet. 2019; 393(10172): 647-654.
- Konopitski A, Okafor C, Smith B, et al. Evolution of total hip arthroplasty in patients younger than 30 years of age: A systematic review and meta-analysis. Archives of Orthopaedic and Trauma Surgery. 2023; 143(2): 1081-1094.
- Shrader MW. Total hip arthroplasty and hip resurfacing arthroplasty in the very young patient. Orthopedic Clinics of North America. 2012; 43(3): 359-367.
- New Zealand Joint Registry. The New Zealand Joint Registry Twenty-Three Year Report January 1999 to December 2021. 2023. https://www.nzoa.org.nz/sites/default/files
- Wilson AE, O’Malley MJ. Total hip Arthroplasty in adolescents and young adults. Operative Techniques in Orthopaedics. 2020; 30(1): 100785.
- Bayliss LE, Culliford D, Monk AP, et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: A population-based Cohort Study. The Lancet. 2017; 389(10077): 1424-1430.
- Jäger M, Begg MJW, Ready J, et al. Primary total hip replacement in childhood, adolescence and young patients: Quality and outcome of clinical studies. Technology and Health Care. 2008; 16(3): 195-214.
- Sedrakyan A, Romero L, Graves S, et al. Survivorship of hip and knee implants in pediatric and young adult populations. Journal of Bone and Joint Surgery. 2014; 96(Suppl 1): 73-78.
- Metcalfe D, Peterson N, Wilkinson JM, et al. Temporal trends and survivorship of total hip arthroplasty in very young patients. Bone Joint J. 2018; 100-B(10): 1320-1329.
- Halvorsen V, Fenstad AM, Engesæter LB, et al. Outcome of 881 total hip arthroplasties in 747 patients 21 years or younger: Data from the Nordic Arthroplasty Register Association (NARA) 1995–2016. Acta Orthopaedica. 2019; 90(4): 331-337.
- Agrawal Y, Kerry RM, Stockley I, et al. Review of total hip arthroplasty in patients younger than 30 years: Mid to long-term results. HIP International. 2021; 31(4): 533-541.
- Stott S, Bidwell T. Epidemiology of slipped capital femoral epiphysis in a population with a high proportion of New Zealand Maori and Pacific children. New Zealand Medical Journal; 2003; 116(1184): U647.
- Sedrakyan A, Graves S, Bordini B, et al. Comparative effectiveness of ceramic-on-ceramic implants in stemmed hip replacement. Journal of Bone and Joint Surgery. 2014; 96(Suppl 1): 34-41.
- Boyle MJ, Frampton CMA, Crawford HA. Early results of total hip arthroplasty in patients with slipped upper femoral epiphysis compared with patients with osteoarthritis. The Journal of Arthroplasty. 2012; 27(6): 1003-1007.
- Dimovski R, Zaltz I. The contemporary role for Hip Arthrodesis in adolescents and young adults. Journal of the Pediatric Orthopaedic Society of North America. 2021; 3(1). DOI: 10.55275/jposna-2021-171.
- Kelman MG, Studdert DM, Callaghan JJ, et al. The choice between total hip arthroplasty and Arthrodesis in adolescent patients: A survey of orthopedic surgeons. The Journal of Arthroplasty. 2016; 31(1): 70-75.
- Puttock DR, Howard DP, Eastley NC, et al. Apparent trends in the use of femoral megaprostheses: An analysis from the National Joint Registry. Arthroplasty; 2022; 4(1): 50.
- Buddhdev PK, Vanhegan IS, Khan T, et al. Early to medium-term outcomes of uncemented ceramic-bearing total hip arthroplasty in teenagers for paediatric hip conditions. Bone Joint J. 2020; 102-B(11): 1491-1496.
- Holmenlund C, Overgaard S, Bilberg R, et al. Evaluation of the oxford hip score: Does it still have content validity? interviews of total hip arthroplasty patients. Health and Quality of Life Outcomes. 2021; 19(1): 237.
- Hannouche D, Devriese F, Delambre J, et al. Ceramic-on-ceramic THA implants in patients younger than 20 years. Clin Orthop Relat Res. 2016; 474(2): 520-527.
