Evaluating the Changes in Sagittal Balance via EOS Imaging before and after Total Hip Arthroplasty
Dariush Dowlat Alizadeh2*, Seyyed Mohammad Jalil Abrisham1, Mohammad Reza Sobhan1
1Department of Orthopedics, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
2Orthopedic Surgery, Trauma Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Abstract
Background and Aim: Sagittal imbalance is often presented as one of the major problems in individuals suffering from orthopedic pain, particularly those affected by destructive hip joint osteoarthritis. In this regard, total hip arthroplasty (THA) as a therapeutic procedure for such patients has resulted in the restoration of sagittal balance. Therefore, the present study aimed to evaluate the changes in sagittal balance using EOS imaging before and after THA and also reflect on its effect on hip joint function, knee pain, and disability percentage due to low back pain (LBP).
Methods: Utilizing a prospective cohort study, a total number of 24 patients suffering from extreme unilateral hip osteoarthritis and in need of unilateral THA were selected based on the inclusion and exclusion criteria, and then, sagittal balance parameters, including pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), sacrofemoral angle (SFA), sacrofemoral distance (SFD), lumbar lordosis (LL), and stem angle (SA) were investigated after performing standing radiographs by means of the EOS device. One year after THA, all the above-mentioned parameters were also measured by EOS imaging before and after the surgery and the patients completed some questionnaires, which is the Oswestry Low Back Pain Disability Index (OLBPDI) to evaluate disability percentage resulting in LBP, the Knee Injury and Osteoarthritis Outcome Score (KOOS) instrument to assess knee pain, and the Harris Hip Score (HHS) measure to rate hip joint function, and then the results were analyzed using the SPSS Statistics software (ver. 17).
Results: The patients consisted of 13 males (54.2%) and 11 females (45.8%) with the mean age of 52.87±13.05. The mean score of the preoperative PI was also equal to 54.74±10.66 and it was 58.19±11.58 after the surgery (p=0.025). However, the mean values of other parameters at the preoperative stage did not show any significant changes. As well, hip joint function and knee pain resulting from LBP improved in the patients after the surgery (p<0.001).
Conclusion: The study findings demonstrated that THA probably influenced sagittal balance through PI. Moreover, the postoperative hip joint function, knee pain, and disability percentage caused by LBP significantly enhanced compared with those before the surgery. Thus, it was concluded that the evaluation of sagittal balance parameters could help patients with orthopedic pain.
Introduction
Degenerative diseases are known as one of the most common orthopedic disorders associated with aging. Hip and knee joints are also among the ones primarily affected by such conditions with their different etiologies. One of the major causes of such diseases is the problem with other parts of the body2,3. In fact, due to the relationship between the pelvis and the spine, any changes in these components can influence the other one. For example, the changes in the pelvic tilt (PT) affect the lumbar lordosis (LL)11,7. In the case of the changes in the pelvis, and then in the LL, patients also experience problems such as hip-spine syndrome.
Following the problems affecting these joints, surgeries such as total hip arthroplasty (THA) can be considered as an option to improve sufferers’ conditions. Actually, when there are indications for surgery, there will be a great deal of focus on better performing it and reducing its subsequent complications. In this regard, it is of utmost importance to reflect on the spatial orientation of the acetabulum during THA, and recruit surgeons with sufficient knowledge of the exact spatial position to the acetabulum to perform THA in order to diminish postoperative discomforts such as a hip dislocation5. For this reason, several techniques are suggested to moderate postoperative complications, including the one developed by Lewinnek, who described the combination of the acetabular inclination and anteversion as a safe zone, and then identified such a zone in the acetabular inclination and anteversion in the total hip arthroplasty, assuming that its observance would decrease the probability of postoperative hip dislocation8,9. However, some studies have so far reported cases of dislocation after primary THA despite much adherence to the safe zone10.
Another procedure, receiving more attention in recent studies, is concentration on sagittal balance5,6. An adequate knowledge of sagittal balance has been accordingly recommended for orthopedic surgeons and neurosurgeons prior to the spine or hip surgeries. In fact, the cooperation among joints, bones, and muscles to create a stable condition in order to stand or walk with the least amount of energy loss has been defined as sagittal balance. Degenerative joint disease in the hip, as well as other problems of the spine, can also change such a balance. Pelvic incidence (PI), as a fixed parameter, and PT and sacral slope (SS), as positional parameters, are thus among the important one shaping sagittal balance. In this sense, PT refers to the angle between the line perpendicular to the sacral plate at its midpoint and the line connecting this point to the femoral head axis, and SS is the tangent line to the superior endplate of S1 and the horizontal plane.
The given parameters can be measured by EOS imaging (an x-ray technology that allows simultaneous acquisition of AP and lateral images of the entire body in a natural, erect position) and used in the formula routinely employed for sagittal balance (i.e., PI = SS + PT).
In fact, surgeons can reduce subsequent complications, such as hip dislocation and impingement by being aware of these parameters and formula. Therefore, this study aimed to investigate the extent of the changes in sagittal balance via EOS imaging before and after THA. At the same time, the status of pain in the back and the hip following THA was examined in the patients to discover whether their knee function changed due to variations in femoral anteversion or not.
Methods
Study Design and Setting
This cohort study was conducted on patients suffering from extreme unilateral hip osteoarthritis, referred to the Specialized Poly-Clinic of Baghaeipour, affiliated to Shahid Sadoughi University of Medical Sciences, Yazd, Iran, from August 2017 to January 2018. All patients had been diagnosed with severe symptomatic unilateral hip joint osteoarthritis included in this study.
Here, extreme hip osteoarthritis meant the severe destruction of the articular surface of the hip with the reduced range of movement and limited daily activities resultant from pain, which had not been treated by physiotherapy or medicines12. The patients with secondary hip osteoarthritis (dysplasia of the hip, rheumatoid arthritis, and ankylosing spondylitis); previous surgery of the hip, or knee; scoliosis with a Cobb angle greater than ten degrees; spondylolisthesis; history of spine fractures; previous bone tuberculosis or any spine infections; excluded from the study. Patients with low back pain which contributed to previous diagnoses specific to spinal stenosis, degenerative disk disease, etc., as well as spinal surgery or neurologic deficit in the lower leg; were also excluded from study.
Using the convenience sampling method, the sample size considering the type-I error of 0.05% and the type-II error of 20% as well as the relative precision of d=1.10 and the average in similar studies was equal to 22 cases3.
Respecting the inclusion and exclusion criteria, there was a total number of 65 patients, including 41 patients excluded from study, i.e., five patients with spine surgery, three patients presenting with previous femur neck surgery and torsion treatment, two patients affected with intertrochanteric femur fractures, three patients with a history of acetabular fracture, and 27 patients with underlying diseases, not referring back to the clinic, and one case due to death. Finally, 24 patients were included in this study.
The patients undergoing THA were treated by a similar surgeon with the same technique of hip direct lateral approach; the Hardinge approach. The non cemented ACTIS Hip Stem by DePuy synthes® was used in all patients.
After prepping and draping, the Hardinge approach were conducted on all patients with a lateral decubitus position. first, by removing the head of femur from the formal acetabulum cutting, the acetabulum was recognized then the acetabular cup was cleared of remaining ligaments and osteophytes and the acetabular articular was trimmed by reamers. According to each patient’s pre-op, the acetabulum was reamed to an optimum size and all patients were determined between 30 and 40 degrees of inclination and 10 degrees of acetabular cup anteversion13.
Upon taking the press-fit measures by two fixed twists and femur preparation based on each patient’s pre-op, the stenting fits in the canal and the stenting femur with 15 degrees of anteversion rather than femur shaft were designed in all patients.
After that, the patients were evaluated considering hip stability. After being confirmed, a drain placed along with the capsule. fascia, muscle, hypoderm, and derma recovered layer by layer.
Due to non-cemented stem conduction, full body weighting started the day after the surgery for patients. All the patients received anticoagulant treatment with heparin and low molecular weight heparin. following that, active and passive movements began after the surgery for next 14 days. All the patients undergo the same physiotherapy protocol and used same medication with NSAIDs after surgery.
The patients undergoing the treatment protocol were treated through the lower extremity alignment using EOS imaging, one week before and one year after THA. All included patients underwent routine biplanar full-body standing stereographs with the EOS system (EOS Imaging Paris, France), a low-dose system acquiring simultaneous stereographs in the sagittal and coronal planes of the patient (with two sources at 90 degrees) from head to toe. Per protocol, images were acquired with the patient standing in the EOS suite in a relaxed position with hands gripping the bar to prevent falling as per manufacturer's guidelines.
Sagittal balance was measured and registered one year before and after the surgery by the EOS device in all 24 patients, and then PI, SS, stem angle (SA), PT, and lumbar lordosis (LL) (S1-L1) were measured at the pre and postoperative stages through EOS and the changes were studied. Moreover, the distance between the sacrum and the center of the femur in millimeter (SFD), the angle between the femur stem and the posterior cortex femur (SA), and the angle of the proximal femur than S1 of the sacrum angle of the upper surface (SFA) were measured and recorded before and after the surgery. (Figure 1, 2, 3)
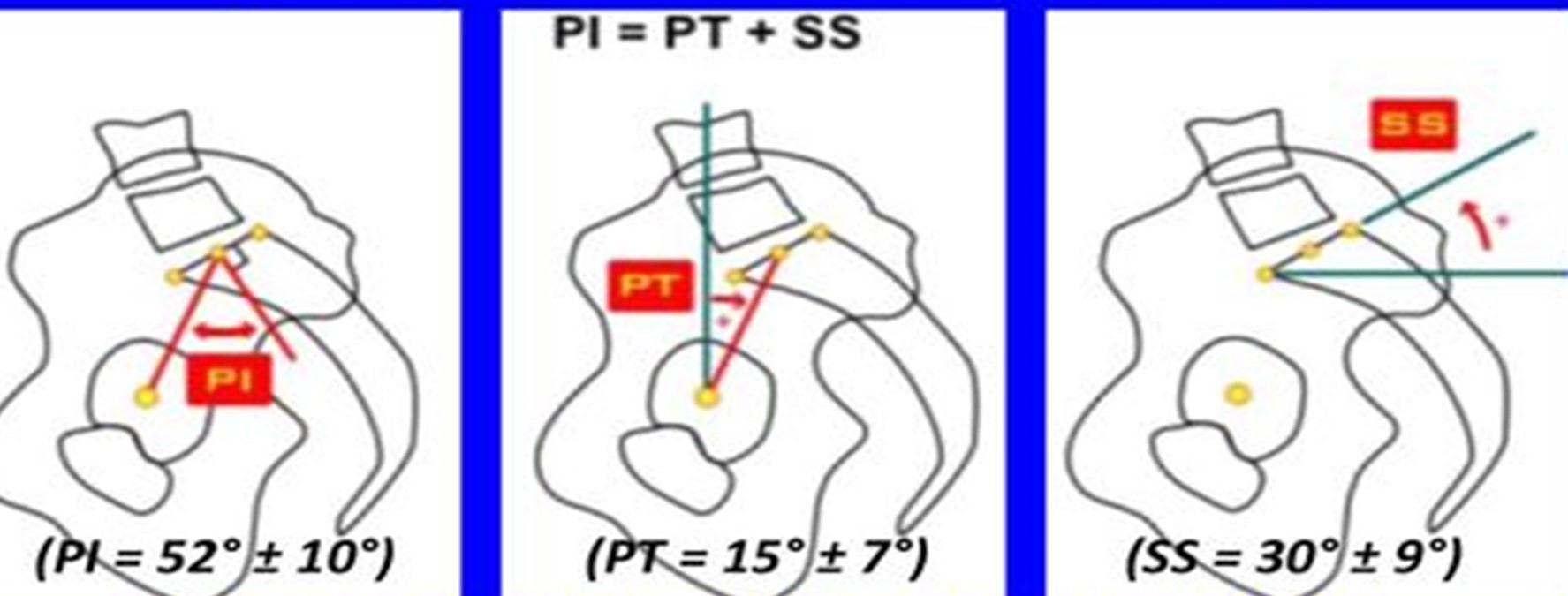
Figure 1: Normal range of splenopelvic parameters. PI pelvic incidence, PT pelvic tilt, SS sacral slope.

Figure 2: Spinopelvic parameters.
LL: Lumbar Lordosis, SFA: Sacro Femoral Angel, SVA: Sagittal Vertical Axis, SFD: Sacro Femoral Distance
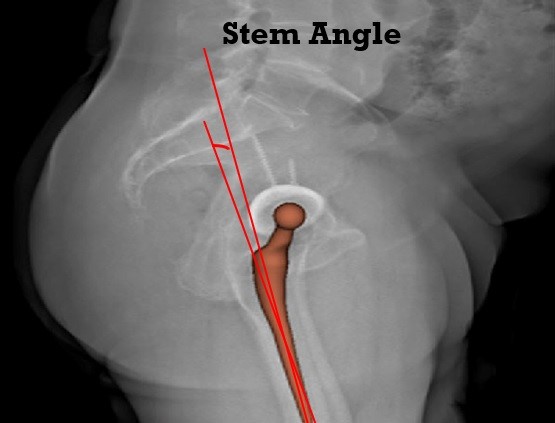
Figure 3: Stem angle.
Of note, these angles and distances were measured by three individuals (except the surgeon and the researcher), including an EOS expert, a resident of orthopedic surgery, and a resident of radiology, and then the average of the sums was recorded in the forms.
In fact, the patients’ information such as age, gender, EOS imaging angles, as well as the data from valid and reliable questionnaires, that is the Oswestry Low Back Pain Disability Index (OLBPDI), the Knee Injury and Osteoarthritis Outcome Score (KOOS) instrument, and the Harris Hip Score (HHS) were completed and recorded before and one year after the surgery for all patients. all data were gathered and analyzed in blind manner.
OLBPDI
The ILBPDI was used to measure the permanent functional disability in patients as a “gold standard” in order to evaluate their back function. In this questionnaire, 10 concepts could be evaluated in patients via several items in each section, including extreme pain, individual protection, lifting, walking, sitting down, standing up, sleeping, marital life, social life, and traveling. The OLBPDI score of level of function corresponds to a percentage of disability whereby a score of 0–20% = minimal disability, 21–40% = moderate disability, 41–60% = severe disability, 61–80% = crippled, and 81–100% = bed bound or exaggerated symptoms15,16.
HHS
The HHS was recruited by a non-treating Physiotherapy Assistant to evaluate the hip surgery results as well as the types of hip joint disabilities and treatment methods1,17. This questionnaire consisted of pain, function, no deformity, and range of movement. The questionnaire was comprised of 10 items with the maximum score of 100. If the HHS scores increased 20 degrees after the surgery and radiology, the surgery results were successful.
KOOS
The KOOS as an international questionnaire was one of the most authentic instruments for the subjective evaluation of knee, using 42 items and five concepts related to patients, such as other symptoms related to the disease (7 items), pain (9 items), daily living activities (17 items), sports and amusement activities (5 items), and quality of life in relation to knee problems (4 items)18,19. The patients' scores could also range from 0 to 100, wherein 100 was the maximum of the problem and 0 demonstrated no problem, that is the lower score of the KOOS meant kind of improvement.
Statistical Analysis
The data were analyzed by an experienced statistical consultant, blinded to the study groups, using the SPSS Statistics software (ver. 17, Chicago, IL, USA). In this sense, mean, standard deviation (SD), frequency, and percentage were employed to report the data. Moreover, Chi-square test (to analyze the qualitative data) and paired-samples t-test (to analyze the quantitative data) or their non-parametric equivalents such as HHS were applied. The p-value was equal to 0.05.
Results
In total, 24 patients, including 13 males (54.2%) and 11 females (45.8%) were included in this study based on the inclusion and exclusion criteria. The mean age of the patients was 52.87±13.05.
The mean values of PI was 54.74±10.66 before the surgery and it was 58.19±11.58 at the postoperative stage (p=0.025). The PI mean scores also augmented in 18 patients (75%) and dropped in six patients (25%) after the surgery (Table 1), but the changes in the mean values of PT, SS, SFA, and SFD, before and after the surgery were not statistically significant (Table 1).
Table 1: Sagittal balance parameters before and after THA
|
|
Frequency |
Mean±SDa |
P-value |
|
PI (before) PI (after) |
24 |
54.74±10.66 |
0.02 |
|
58.19±11.58 |
|||
|
PT (before) PT (after) |
24 |
11.29±6.19 |
0.21 |
|
15.93±17.04 |
|||
|
SS (before) SS (after) |
24 |
46.88±9.59 |
0.63 |
|
47.50±11.61 |
|||
|
SFAb (before) SFA (after) |
24 |
21.46±10.37 |
0.54 |
|
22.37±11.68 |
|||
|
SFDc (before) SFD (after) |
24 |
13.70±13.32 |
0.93 |
|
13.77±14.16 |
aStandard deviation, bSacrofemoral angle, cSacrofemoral distance
Moreover, PI was compared among males and females after the surgery, and it was respectively 62.11±12.74 and 54.88±9.79 among the female and male patients, which did not show a significant difference between both groups. As well, there was no significant difference after the surgery between males and females respecting PT, SS, SFA, and SFD mean scores (Table 2).
Table 2: Sagittal balance parameters after THA
|
|
Gender |
Frequency |
Mean±SDa |
Total |
P-value |
|
PI (after) |
Male |
13 |
54.88±9.79 |
24 |
0.13 |
|
Female |
11 |
62.11±12.74 |
|||
|
PT (after) |
Male |
13 |
12.09±5.70 |
24 |
0.23 |
|
Female |
11 |
20.46±24.24 |
|||
|
SS (after) |
Male |
13 |
45.19±14.35 |
24 |
0.27 |
|
Female |
11 |
50.24±6.92 |
|||
|
SFAb (after) |
Male |
13 |
21.52±13.14 |
24 |
0.7 |
|
Female |
11 |
23.38±10.23 |
|||
|
SFDc (after) |
Male |
13 |
13.91±1.89 |
24 |
0.96 |
|
Female |
11 |
13.61±13.97 |
|||
|
SAd (after) |
Male |
13 |
6.37±2.67 |
24 |
XXX |
|
Female |
11 |
6.02±2.84 |
aStandard deviation, bSacrofemoral angle, bSacrofemoral distance, dStem angle
In this study, the OLPBDI, KOOS, and HHS were used to evaluate the patients before and after the surgery, indicating that the patients' status statistically improved (Table 3) (Figure 4).
Table 3: KOOS, HHS, and OLBPDI scores before and after THA
|
|
Frequency |
Mean±SDa |
P-value |
|
KOOSb (before) KOOS (after) |
24 |
25.28±8.19 |
<0.0001 |
|
18.64±7.37 |
|||
|
HHSc (before) HHS (after) |
24 |
24.50±10.90 |
<0.0001 |
|
90.45±4.75 |
|||
|
OLBPDI (before) OLBPDI (After) |
24 |
46.91±36.10 |
0.003 |
|
7.83±5.74 |
aStandard deviation, bKnee Injury and Osteoarthritis Outcome Score, cHarris Hip Score, dOswestry Low Back Pain Disability Index
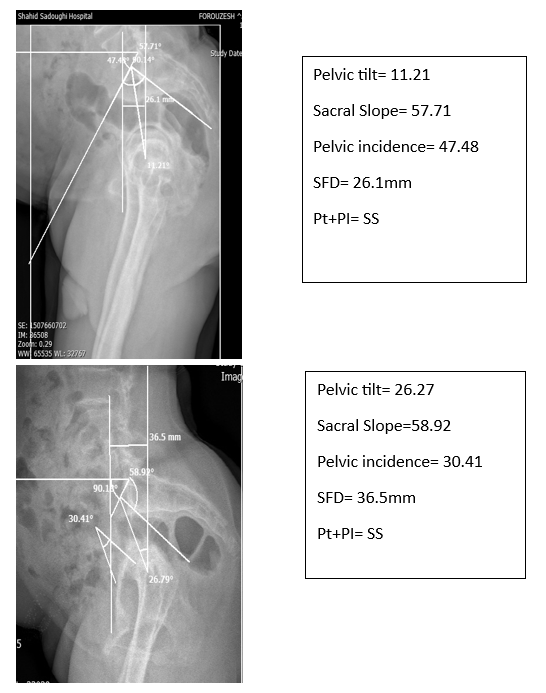
Figure 4: Comparison of two patients with different spinopelvic parameters.
Discussion
The main purpose of this study was to evaluate the changes in sagittal balance using EOS imaging before and after THA and also reflect on the effect of THA on hip joint function, knee pain, and disability percentage due to LBP. The study results established that THA affected sagittal balance. In fact, THA changed the hip angles. However, the changes in PT and SS were not significant compared with those before the surgery, but the whole changes led to some considerable changes in PI. In addition, the little changes in SS resulted in some slight changes in LL, which were not significant. Moreover, hip joint function, knee pain, and disability percentage induced by LBP improved at the postoperative stage that are concluded by patients judgment among questionaries assessment.
In this line, Ochi et al. in a prospective study had investigated 74 patients treated with THA in terms of their hip medullary balance and the changes observed in all four parameters (which are PT, SS, LL, and PI) had been somehow consistent with the results of the present study except for PI, which was significant11. Totally, both studies were comparable since PI had been affected by PT and SS and the changes in these two parameters had directly influenced PI, and also we believe that this is justifiable when you consider another parameter as SFD which is also related to PI changes. SFD is not considered in Ochi et al. study.
In fact, although the changes in PT and SS were not statistically significant, they were clinically important and able to give rise to pain and hip instability14.
In an article published by Staibano et al. the effect of total joint arthroplasty on LBP was studied. In this prospective cohort study the prevalence of significant preoperative LBP, as identified by the patient and reported as moderate to worst imaginable pain on the Oswestry Disability Index, was significantly high among hip patients with 28.8% reporting LBP21.
In a study by Piaazzolla et al. in 2017, the improvement of spinopelvic parameter changes and LBP after unilateral THA was investigated and they suggested that the spinopelvic misalignment observed in patients with concomitant unilateral hip osteoarthritis and LBP, in the absence of spine structural pathologies, reflects an antalgic posture developed by the patients to keep spine as vertical as possible. After THA, a significant increase of PT and a significant reduction of SS, LL are recorded20.
Besides, a slight increase in these two parameters could be one of the elements in alleviating pain in most of the patients suffering from LBP. As well, Weng et al. had observed 39 patients undergoing THA for one year and found that LBP had been completely improved in 17 cases and pain had been minimized in 22 patients. These results were in harmony with the findings reported in the present study. It was thus concluded that hip problems could make some changes in an individual’s sagittal balance and have direct effects on their LBP, so it was possible to relieve their pain by eliminating the hip problems and correcting sagittal imbalance.
In addition, Weng et al. had observed that THA could have a non-significant effect on PT, LL, and SS, while investigating patients’ sagittal balance. Actually, these parameters had slightly elevated compared with those before the surgery, but they were not statistically significant, which was in conflict with the results of the present study. Correspondingly, PI had experienced small changes, not supporting those in the present study14.
Moreover, Legaye had observed that PI improvement could alleviate LBP in 200 patients in line with the findings reported in the present study, denoting that PI improvement after THA could mitigate patients’ backache.
Kechagias et al. had also researched sagittal balance in the hip and the spine during LBP, after THA in 2019 and found improvement in the status of patients' sagittal balance. In the present study using THA, the KOOS instrument mean score had demonstrated a significant change than that before the surgery, so it was concluded that THA was probably able to significantly help patients relieve their pain such as knee pain with a small change in patients’ balance22.
Nevertheless, observing 28 patients with spinal column disorders undergoing THA during six months, Eyvazov et al. had observed no consistency between the changes in balance and LBP. They had also maintained that LPB alleviation after THA was not correlated with sagittal balance13. As well, Radcliff et al. had investigated two groups of patients, suffering from LBP and non-sufferers, and found that unilateral THA could help them with their pains by improving SS and LL4.
But finally, no changes had been detected in SS and LL in these patients and there had been no significant changes in the spinal column pain following unilateral THA after nine months, which were not consistent with the results of the present study.
Investigating knee pain before and after surgery was one of the differences between this study and other similar ones, wherein the relative improvement demonstrated that THA affected knee pain, and these results were in agreement with the reports by Ben-Galim et al, establishing the advantages of THA on LBP after two years1.
On the other hand, PI was equal to the total sum of PT and SS (PI=PT+SS) This equation holds true in any time, but not so in six patients, we are suggesting this may be related to the radiographic technique rather than to the true clinical posture or gait or measurement errors.
In addition, the distance between the center of the hip to the sacrum (SFD) before and after the surgery compared in all patients showed no significant changes. As well, the angle between the sacrum and the femur investigated before and after the surgery in all patients revealed no significant changes.
As it was expected that PT was improved and SFD was reduced by THA, this distance did not indicate much difference due to the unilaterality of the surgery. Another reason was associated with the inconsistency of PT among the patients (they may have Antivert or retrovert pelvic) or even the short duration of the follow-up. Moreover, it was expected that SFA would drop following the modification of the acetabulum problem and the reduction of the PT-induced psoas syndrome, but in action it did not occur and it was not statistically significant, maybe due to the wrong physiotherapy course in the patients. Besides, it was believed SA with the posterior femur was effective in reducing patients’ pain in all angles and improving hip movements, as it occurred but not equally. Extremity pain and inconsistency in sagittal balance (in patients with Antivert or retrovert pelvic) had thus distorted the effect of this parameter, demanding a more coherent patient population.
Moreover, this hypothesis was proposed that in patients suffering from degenerative hip and spine diseases undergoing surgeries, the posterior fusion of the spinal column before the surgery could improve sagittal balance. As well, in patients treated with THA before the spinal fixation, lower extremity alignment and attention to the changes in the acetabulum and back angles needed to be evaluated to help patients moderate the undesired effects of hip fractures18.
This study had some limitations, such as patients not cooperating in EOS imaging and simultaneous CT scans before and after the surgery and in the follow-up. It is thus recommended to conduct similar studies with a larger sample size and increase follow-up duration even to five or even 10 years after the surgery. This study has to be investigated in patients with bilateral hip osteoarthritis, to assess the role of bilateral versus unilateral THA on the sagittal balance. Furthermore, the angles should be investigated in healthy people.
Conclusion
The study results revealed that the three parameters of SS, PT, and LL boosted in value, but not significantly, due to some changes in PI at the preoperative stage; so it was concluded that THA affected sagittal balance. Moreover, hip joint function, knee pain, and disability percentage resultant from LBP improved significantly compared with the conditions before the surgery. We concluded that the management of patients with hip osteoarthritis also manages their LBP, but it should be considered that the improvement in SS and LL and hip motion might also contribute to the relief of LBP.
Ethics
The main purpose of this study was accurately explained to the patients and the probable consequences were also mentioned. No offensive action was done on the patients. A documented consent form was then obtained from the patients and this project was approved by the Ethics Committee of Shahid Sadoughi University of Medical Sciences, Yazd, Iran (Ethics code: IR.SSU.MEDICINE.REC.1397.008). As well, the confidentiality of patient information and the moral codes related to human studies based on the Declaration of Helsinki were considered.
Disclosure Statement
The authors declare no conflict of interest in this study.
References
- Ben-Galim P, Ben-Galim T, Rand N, et al. Hip-spine syndrome: the effect of total hip replacement surgery on low back pain in severe osteoarthritis of the hip. Spine. 2007; 32(19): 2099-102.
- McAuley JP, Szuszczewicz ES, Young A, et al. Total hip arthroplasty in patients 50 years and younger. Clin Orthop Relat Res. 2004; (418): 119-25.
- Kim YH, Kim JS, Park JW, et al. Contemporary total hip arthroplasty with and without cement in patients with osteonecrosis of the femoral head: a concise follow-up, at an average of seventeen years of a previous report. J Bone Joint Surg Am. 2011; 93(19): 1806-10.
- Radcliff KE, Orozco F, Molby N, et al. Change in spinal alignment after total hip arthroplasty. Orthopaedic surgery. 2013; 5(4): 261-5.
- Legaye J. Influence of the sagittal balance of the spine on the anterior pelvic plane and on the acetabular orientation. International orthopaedics. 2009; 33(6): 1695-700.
- Lugade V, Klausmeier V, Jewett B, et al. Short-term recovery of balance control after total hip arthroplasty. Clinical orthopaedics and related research. 2008; 466(12): 3051.
- Shon WY, Sharma V, Moon JG, et al. Can pelvic tilting be ignored in total hip arthroplasty? International journal of surgery case reports. 2014; 5(9): 633-6.
- Lazennec J, Riwan A, Gravez F, et al. Hip spine relationships: application to total hip arthroplasty. Hip international: the journal of clinical and experimental research on hip pathology and therapy. 2006; 17: S91-104.
- Zhan C, Kaczmarek R, Loyo-Berrios N, et al. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am. 2007; 89(3): 526-33.
- Siopack JS, Jergesen HE. Total hip arthroplasty. West J Med. 1995; 162(3): 243-9.
- Ochi H, Baba T, Homma Y, et al. Importance of the spinopelvic factors on the pelvic inclination from standing to sitting before total hip arthroplasty. European Spine Journal. 2016; 25(11): 3699-706.
- Quintana JM, Arostegui I, Escobar A, et al. Prevalence of knee and hip osteoarthritis and the appropriateness of joint replacement in an older population. Archives of internal medicine. 2008; 168(14): 1576-84.
- Eyvazov K, Eyvazov B, Basar S, et al. Effects of total hip arthroplasty on spinal sagittal alignment and static balance: a prospective study on 28 patients. European Spine Journal. 2016; 25(11): 3615-21.
- Weng W, Wu H, Wu M, et al. The effect of total hip arthroplasty on sagittal spinal–pelvic–leg alignment and low back pain in patients with severe hip osteoarthritis. European Spine Journal. 2016; 25(11): 3608-14.
- Fairbank JCT, Pynsent PB. The Oswestry Disability Index. Spine. 2000; 25(22): 2940-2953.
- Davidson M, Keating J. A comparison of five low back disability questionnaires: reliability and responsiveness. Physical Therapy. 2002; 82: 8-24.
- Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000; 25(22): 2940-52.
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am.1969;51: 737-55.
- Saraie Pour S, Salavati M, Akhbari B, et al. Translation and adaptation of knee injury and osteoarthritis outcome score (KOOS) in to persian and testing persian version reliabilitation among Iranians with osteoarthritis. 2007; 1(28): 42-46.
- Piazzolla A, Solarino G, Bizzoca D, et al. Spinopelvic parameter changes and low back pain improvement due to femoral neck anteversion in patients with severe unilateral primary hip osteoarthritis undergoing total hip replacement. European Spine Journal. 2018; 27: 125-134.
- Staibano P, Winemaker M, Petruccelli D, et al. Total joint arthroplasty and preoperative low back pain. The Journal of arthroplasty. 2014; 29(5): 867-871.
- Kechagias VA, Grivas TB, Papagelopoulos PJ, et al. Truncal changes in patients after total hip or knee arthroplasty: a surface topography study. Cureus. 2019; 11(3): e4260.
