Transolecranon Distal Humerus Fractures: A Mini Review
Shaan S. Patel*, Julian Gatta, Adrienne Lee, Blaine T. Bafus
Department of Orthopaedic Surgery, MetroHealth Medical Center, Cleveland, OH, USA
Abstract
Background: Transolecranon distal humerus fractures are uncommon injuries. The purpose of this study is to review the outcomes and complications associated with transolecranon distal humerus fractures.
Material and Methods: We performed a systematic search of PubMed for articles published between 1990 and 2021. Included studies reported outcomes and complications of transolecranon distal humerus fractures. Data was extracted from the included studies to describe patient demographics, injury characteristics, outcome measurements, and complications.
Results: A total of 4 studies met inclusion criteria for data extraction and analysis. Two studies evaluated an adult cohort of a total of 18 patients. The average Disabilities of the Arm, Shoulder, and Hand (DASH) score was 40 (range 4.2 – 76.5). Fifteen patients (83%) had a complication. Elbow stiffness (11/18, 61%) was the most common complication. Eleven patients (61%) underwent more than one procedure. Two studies evaluated a pediatric cohort of a total of 9 patients. Five patients (56%) underwent non-operative treatment with immobilization and four patients (44%) underwent open reduction and internal fixation. There were no complications reported. All the pediatric patients regained near full range of motion of the elbow at their final follow-up.
Conclusion: Transolecranon distal humerus fractures are complex elbow injuries. In the adult population, they remain a challenge for orthopaedic surgeons. Complications, including elbow stiffness and infection, are high with frequent long-term functional limitations as represented by DASH scores. In contrast, pediatric patients have good outcomes and minimal complications that are similar to isolated olecranon and distal humerus fractures in children.
Background
Transolecranon distal humerus fractures are high-energy, traumatic injuries1. The mechanism of injury is an axial load of the distal humerus through the olecranon resulting in both distal humerus and olecranon fractures (Figure 1). The distal humerus fracture is usually intra-articular and multi-fragmentary and the olecranon fracture can extend to the coronoid or proximal ulnar diaphysis2. The incidence of this fracture pattern is unknown. This is likely because there is no specific classification scheme for this injury.
Outcomes of transolecranon fracture-dislocations3-6 and isolated distal humerus fractures7-15 have been described in the literature. The purpose of this study was to review the outcomes and complications associated with transolecranon distal humerus fractures.

Figure 1: Radiographs of a transolecranon distal humerus fracture. The AP (a) and lateral (b) views of the elbow demonstrate the multi-fragmentary distal humerus and olecranon fractures. The AP (c) and lateral (d) views of the elbow show internal fixation of the distal humerus and olecranon that went on to fracture nonunion secondary to infection.
Materials and Methods
To identify relevant publications, we searched PubMed, including studies from 1990 to February 2021. The literature search was limited to studies since 1990 to ensure findings reflected modern clinical practices and implants. We searched for terms “transolecranon fracture”, “distal humerus fracture”, “olecranon fracture”, “proximal ulna fracture”, and “transolecranon distal humerus fracture”. The following were the inclusion criteria: 1) the study population included pediatric or adult patients with transolecranon distal humerus fractures, 2) outcome measurements were obtained through clinical exam (e.g., range of motion) or questionnaires (e.g., Disabilities of the Arm, Shoulder, and Hand), 3) complications, if any, were reported for the study population. If a study had a subpopulation that met the inclusion criteria, the study was included. One reviewer applied the inclusion criteria to the studies gathered from the PubMed search, determined which studies to include in the review, and extracted the data from each study. Data that was extracted included patient demographics, injury characteristics, outcome measurements, and complications. Descriptive statistics were reported as means and range for continuous variables and as counts and percentages for categorical variables for patient demographics, outcome measurements, and complications. The Oxford Centre for Evidence-Based Medicine was used to assess the level of evidence for each included study16.
Results
The search for relevant studies was initiated in February 2021 (Figure 2). Four studies met inclusion criteria for data extraction and were level 4 evidence16. There was one case series1 and one case report17 of adult patients with transolecranon distal humerus fractures. There was one case series18 and one case report19 of pediatric patients with transolecranon distal humerus fractures. There were two case series that had three total patients with transolecranon distal humerus fractures3,6. However, they did not report outcomes or complications of this subpopulation and were not included in this review.
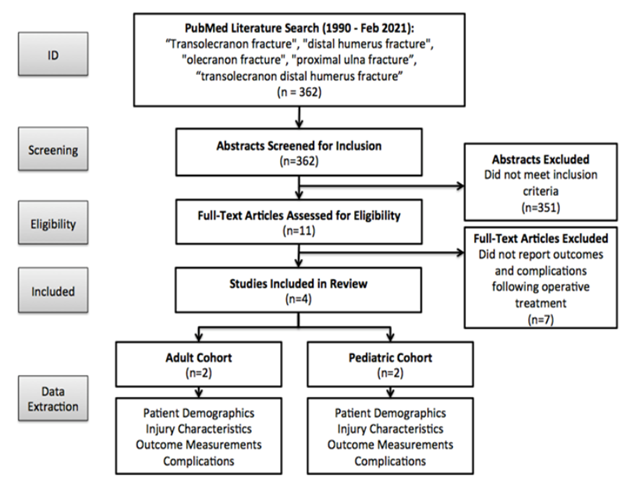
Figure 2: Flow diagram of the PubMed literature search and identification of studies to include in the review
Adult Cohort
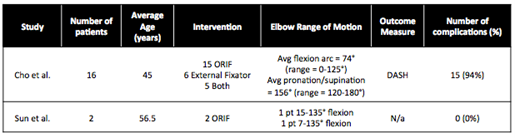
Cho et al. (Cho)1 had a case series of 16 adult patients and Sun et al. (Sun)17 had a case report of 2 adult patients with transolecranon distal humerus fractures (Table 1). Among the two studies, the average age was 46 years (range 20 – 92 years) with 11 females (61%). The dominant extremity was fractured in 7 patients (39%). Thirteen patients (72%) had high-energy mechanisms of injury. Seven patients (39%) were polytrauma patients. Twelve of the fractures (67%) were open with five being grade III open injuries20. Fractures of the distal humerus were classified using the AO/Orthopaedic Trauma Association (OTA) classification21. Seven patients (39%) had C-type fractures. Eight patients (44%) had B-type fractures. Three patients (17%) had A-type fractures.
All patients eventually underwent open reduction internal fixation as definitive treatment for their fracture except for one patient in Cho’s case series. The average clinical follow-up among the 18 adult patients was 16.6 months (range 3.4 – 52.4 months). In Cho’s cohort1, the average extension-flexion arc was 74 degrees (range 0 – 125 degrees) and average pronation-supination arc was 156 degrees (range 120 – 180 degrees). Cho1 reported Disabilities of the Arm, Shoulder, and Hand (DASH) scores for 10 patients. At an average of 3.8 years from the date of injury, the average DASH score was 40.2 (range 4.2 – 76.5). Sun17 did not have patient-reported outcome measurements. However, they did report range of motion of the elbow for their two patients at the final 2-year follow-up. One patient had active range of motion of 15 to 135 degrees extension-flexion, and the second patient had active range of motion of 7 to 133 degrees extension-flexion.
Complications were observed in 15 adult patients (83%) among the two studies. Cho1 reported elbow stiffness, defined as an arc of elbow flexion/extension less than 100 degrees, in 11 patients (61%). Three patients (17%) underwent contracture release. Seven patients (39%) developed deep infections and underwent surgical debridement and intravenous antibiotics. All infections were successfully treated with surgical debridement and antibiotics. Wound dehiscence occurred in 4 patients (22%). Two patients (11%) underwent flap reconstruction with a bipedicle flap and a posterior interosseous island flap. Eight patients (44%) had an ulnar nerve palsy post-operatively and two patients (11%) underwent additional surgery for the ulnar neuropathy. The remaining six patients (33%) had resolution of their ulnar nerve palsy with conservative management. Heterotopic ossification (HO) that was clinically relevant and causing functional limitations, based on Hastings and Graham classification22, was present in 7 patients (39%). Four patients (22%) developed post-traumatic arthrosis and one patient (6%) underwent additional surgery with excision of osteophytes. There were 7 patients (39%) with fracture nonunion, 5 of the olecranon and 2 of the distal humerus. Two patients (11%) underwent repair of the nonunion. Overall, eleven patients (61%) underwent more than 1 surgery to manage their injuries. Sun17 did not report any complications among their two patients at final 2-year follow-up.
Pediatric Cohort
Sharma et al. (Sharma)18 had a case series of 8 pediatric patients and Farooq et al. (Farooq)19 had a case report of 1 pediatric patient with transolecranon distal humerus fractures (Table 1). Among the two studies, the average age was 4.1 years (range 3 – 7 years) with 3 females (33%). Mechanism of injury was reported for one patient in Farooq’s case report19, which was high-energy. All patients had a distal humerus lateral condyle fracture with an olecranon fracture. Two patients (22%) had displaced lateral condyle and olecranon fractures and underwent open reduction and internal fixation with Kirschner wires. Two patients (22%) had displaced lateral condyle fractures and non-displaced olecranon fractures and underwent open reduction and internal fixation with Kirschner wire (n=1) or screw fixation (n=1) of the lateral condyle fracture only. Five patients (56%) had non-displaced olecranon and lateral condyle fractures and underwent non-operative treatment with immobilization.
The patient in Farooq’s case report19 followed up for 6 months after operative fixation of the displaced olecranon and lateral condyle fractures. The patient had 0 degrees elbow extension and 130 degrees elbow flexion with 70 degrees pronation and 80 degrees supination at final follow-up. There was union of the fractures and no complications. Sharma’s case series18 of 8 patients had 7 excellent results and 1 good result based on Flynn criteria23. The range of motion of the patients were not reported in the study. The patient, who underwent operative fixation of displaced olecranon and lateral condyle fractures, had 10 degrees loss of terminal extension. Otherwise, there were no complications.
Table 1: Summary of Studies in the Review
Adult Cohort
Pediatric Cohort
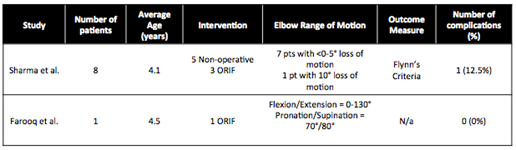
Avg = Average; DASH = Disabilities of the Arm, Hand, and Shoulder; ORIF = Open Reduction and Internal Fixation; pt(s) = patient(s)
Discussion
Transolecranon distal humerus fractures are complex injuries, especially in the adult population. This review illustrated the paucity of literature about this challenging elbow injury. There were 4 total studies (2 adult and 2 pediatric cohorts) evaluating the outcomes and complications of transolecranon distal humerus fractures1,17-19.
Among the adult population, transolecranon distal humerus fractures were associated with high-energy mechanisms of injury with extensive soft tissue disruption. In this review of transolecranon distal humerus fractures, there was a complication rate of 83% in the adult cohort. Elbow stiffness of less than 100 degrees arc of motion was the most common complication (11/18, 61%). Infection, nonunion, and heterotopic ossification occurred in about 40% (7/18) of the patients. The nonunion rate may have been high due to the high rate of open fractures, articular injury, and soft tissue disruption. Use of radiation and NSAIDs for heterotopic prophylaxis may be considered for all patients without contraindications, or selectively in patients with elevated risk, such as those with open fractures and traumatic brain injury. Sixty-one percent of the patients (11/18) underwent more than one surgery. These complications were higher than isolated olecranon fractures, distal humerus fractures, or transolecranon fracture-dislocations2,3,6,8,13,15,25. Also, distal humerus fractures and elbow fracture-dislocations are known to be a common source of post-traumatic elbow arthrosis due to greater severity of articular surface injury3,24. There were 4 patients (22%) who developed post-traumatic arthrosis. This may have been an underestimate as the radiographic follow-up in the two studies was less than 1 year. The average DASH score of 40 illustrated the everyday impairment adult patients experienced as a result of this injury.
Among the pediatric population, transolecranon distal humerus fractures had better outcomes. The patients in this review were not polytrauma patients, did not have open fractures, and had average age of 4. Therefore, the mechanism of injury was likely lower energy and did not have extensive soft tissue injuries unlike the adult cohort. Five patients were treated non-operatively for non-displaced fractures and four patients were treated with operative fixation. One patient had displaced olecranon and lateral condyle fractures and underwent operative fixation. He had 10 degrees loss of terminal extension. Otherwise, there were no reported complications. These outcomes were similar to isolated olecranon and lateral condyle fractures in the pediatric population26,27.
There were limitations of this review. The strength of the review was dependent on the quality of the included studies. The review only had case series and case reports, which are level 4 evidence16. The review only included retrospective studies, so there were inherent weaknesses, including loss to follow-up, differences in surgical technique, and post-operative rehab between the studies. The patient follow-up among the studies were inconsistent with some patients lacking long-term follow-up. All the studies in the review did not provide the same outcome measures. The studies in the review were published over a 12-year span (2009 to 2021) and may represent different surgical procedures. However, this is not a significant limitation. The two adult studies1,17 were published in 2019 and 2021 and used modern implants for fixation of distal humerus and olecranon fractures in adults. The two pediatric studies were published in 2009 and 2016. The pediatric fractures were treated non-operatively or operatively with Kirschner wires or screw fixation, which is the same surgical procedure that would be performed today.
Transolecranon distal humerus fractures are complex elbow injuries. In adult patients, they have high rates of elbow stiffness, infection, nonunion, and functional limitations. Surgeons and patients should be made aware of the high rates of complications and loss of elbow function. On the other hand, pediatric patients have good outcomes and minimal complications that are similar to isolated olecranon and distal humerus fractures in children. Future research on transolecranon distal humerus fractures need to focus on the adult population. There needs to be higher level of evidence studies evaluating post-operative rehab protocols to improve elbow stiffness, wound management and antibiotics to reduce infection rates, and fixation strategies to increase union rates.
Conflicts of Interest
Blaine T. Bafus has the following disclosures:
American Society for Surgery of the Hand: Board or committee member
Polynovo LTD: Stock or stock Options
Shaan S. Patel, Julian Gatta, and Adrienne Lee do not have any disclosures. All authors contributed to the conception and design of the study, data analysis, manuscript writing and editing.
Funding
None
References
- Cho E, Weber MB, Opel D, et al. Complications and functional outcomes after transolecranon distal humerus fracture. J Shoulder Elbow Surg. 2021; 30(3): 479-486.
- Chan K, King GJW, Faber KJ. Treatment of complex elbow fracture-dislocations. Curr Rev Musculoskelet Med. 2016; 9(2): 185-189.
- Haller JM, Hulet DA, Hannay W, et al. Patient outcomes after transolecranon fracture-dislocation. J Am Acad Orthop Surg. 2021; 29(3): 109-115.
- Mouhsine E, Akiki A, Castagna A, et al. Transolecranon anterior fracture dislocation. Journal of Shoulder and Elbow Surgery. 2007; 16(3): 352-357.
- Mortazavi SMJ, Asadollahi S, Tahririan MA. Functional outcome following treatment of transolecranon fracture-dislocation of the elbow. Injury. 2006; 37(3): 284-288.
- Ring D, Jupiter JB, Sanders RW, et al. Transolecranon fracture-dislocation of the elbow. J Orthop Trauma. 1997; 11(8): 545-550.
- Varecka TF, Myeroff C. Distal humerus fractures in the elderly population. Journal of the American Academy of Orthopaedic Surgeons. 2017; 25(10): 673-683.
- Patel SS, Mir H, Horowitz E, et al. ORIF of distal humerus fractures with modern pre-contoured implants is still associated with a high rate of complications. Indian J Orthop. 2020; 54(5): 570-579.
- Robinson CM, Hill RM, Jacobs N, et al. Adult distal humeral metaphyseal fractures: epidemiology and results of treatment. J Orthop Trauma. 2003; 17(1): 38-47.
- Kundel K, Braun W, Wieberneit J, et al. Intraarticular distal humerus fractures. Factors affecting functional outcome. Clin Orthop Relat Res. 1996; (332): 200-208.
- Gofton WT, Macdermid JC, Patterson SD, et al. Functional outcome of AO type C distal humeral fractures. J Hand Surg Am. 2003; 28(2): 294-308.
- Athwal GS, Hoxie SC, Rispoli DM, et al. Precontoured parallel plate fixation of AO/OTA type C distal humerus fractures. J Orthop Trauma. 2009; 23(8): 575-580.
- Ring D, Jupiter JB. Complex fractures of the distal humerus and their complications. J Shoulder Elbow Surg. 1999; 8(1): 85-97.
- Mckee MD, Wilson TL, Winston L, et al. Functional outcome following surgical treatment of intra-articular distal humeral fractures through a posterior approach. J Bone Joint Surg Am. 2000; 82(12): 1701-1707.
- Doornberg JN, Van duijn PJ, Linzel D, et al. Surgical treatment of intra-articular fractures of the distal part of the humerus. Functional outcome after twelve to thirty years. J Bone Joint Surg Am. 2007; 89(7): 1524-1532.
- “Oxford Centre for Evidence-Based Medicine: Levels of Evidence”. University of Oxford: Centre for Evidence-Based Medicine. March 2009. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009
- Sun Y, Thanomsingh P, Jeon I-H. Coronal shear fracture of distal humerus associated with olecranon fracture: A case report and pathomechanism. J Orthop Surg (Hong Kong). 2019; 27(2): 2309499019849707.
- Sharma H, Sibinski M, Sherlock DA. Outcome of lateral humeral condylar mass fractures in children associated with elbow dislocation or olecranon fracture. Int Orthop. 2009; 33(2): 509-514.
- Farooq M, Kamal Y, Ahmad Khan H, et al. Concurrent lateral condyle mass fracture with olecranon fracture: a case report and brief review of literature. Arch Trauma Res. 2016; 5(3): e24760.
- Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984; 24: 742-6.
- Muller ME. The comprehensive classification of fractures of long bones. In: Muller ME, Allgower M, Schneider R, et al., eds. Manual of Internal Fixation. 3rd ed. Berlin: Springer-Verlag. 1991: 118–150.
- Hastings H, Graham TJ. The classification and treatment of heterotopic ossification about the elbow and forearm. Hand Clin. 1994; 10: 417-37.
- Flynn JC. Nonunion of slightly displaced fractures of the lateral humeral condyle in children: an update. Journal of Pediatric Orthopaedics. 1989; 9(6): 691-696.
- Guitton TG, Zurakowski D, van Dijk NC, et al. Incidence and risk factors for the development of radiographic arthrosis after traumatic elbow injuries. J Hand Surg Am. 2010; 35: 1976-80.
- Hak DJ, Golladay GJ. Olecranon fractures: treatment options. Journal of the American Academy of Orthopaedic Surgeons. 2000; 8(4): 266-275.
- Abzug JM, Dua K, Kozin SH, et al. Current concepts in the treatment of lateral condyle fractures in children. J Am Acad Orthop Surg. 2020; 28(1): e9-e19.
- Graves SC, Canale ST. Fractures of the olecranon in children: long-term follow-up. J Pediatr Orthop. 1993; 13(2): 239-241.
