Sex-specific Considerations for Shoulder Instability and Adhesive Capsulitis in Females
Kathryn A. Barth, Claire D. Eliasberg, Karen M. Sutton*
Department of Orthopedic Surgery, Hospital for Special Surgery, New York, NY, USA
Abstract
There has been an increasing focus on sex-specific differences within the context of sports medicine. Differences exist between the sexes leading to disparities in the types of injuries female athletes sustain and the rates at which they experience them. Recognition and awareness of subtle differences between the sexes can lead to a more nuanced diagnosis and treatment of such injuries. The purpose of this study is to review shoulder pathologies that are relevant to the female athlete, specifically adhesive capsulitis, multidirectional instability, and traumatic unidirectional shoulder instability, and highlight the differences in diagnosis, treatment, and outcomes between the sexes. Women suffer from adhesive capsulitis at a greater rate than men and there are risk factors such as breast cancer surgery that are unique to women. Females are much more likely to experience atraumatic shoulder instability than their male counterparts. While females represent a minority of patients who suffer traumatic unidirectional shoulder instability, they should not be overlooked with regards to this condition. There are challenges related to the diagnosis and treatment of these pathologies that are distinctive to female athletes.
Introduction
There has been increased focus on sex-specific differences in sports medicine, specifically with regards to prevention, presentation, and management of athletic injuries. Anatomic, biomechanical, hormonal, and psychologic differences exist between the sexes leading to disparities in the types of injuries female athletes sustain and the rates at which they experience them. Women are more susceptible to overuse injuries and among directly comparable sports, they are more likely than men to sustain injuries requiring surgical management1. These differences have been described in the hip, knee, and ankle, and the shoulder is no exception2. The purpose of this study is to highlight shoulder pathologies that have some sex-specific differences and review the approach to diagnosis, treatment, and outcomes.
Adhesive Capsulitis
Genetics and Sex-Specific Risk Factors
Adhesive capsulitis is a morbid condition that can lead to substantial functional loss and impairment in activities of daily living. It occurs in 2-5% of the population but disproportionately affects women with a male to female ratio reported between 1:1.5 and 1:1.83-5. Other risk factors include diabetes mellitus, autoimmune diseases, cerebral vascular accidents, myocardial infarctions, and recent surgery6. Furthermore, females with adhesive capsulitis tend to have a higher intensity of shoulder pain than males7.
In addition to a female predominance, there appears to be a genetic link to adhesive capsulitis. A study of 1,828 female twin pairs demonstrated the hereditability of adhesive capsulitis to be 42%, while another study found the relative risk for adhesive capsulitis among those with a first degree relative with condition to be 4:13,4,8,9. Having a first- or second-degree relatives from the British Isles is also a risk factor for adhesive capsulitis, further suggesting a genetic link3. Moreover, studies show higher rates of HLA B27 positivity in patients with adhesive capsulitis compared to controls. HLA B27 is thought to trigger an inflammatory response, which may be contributing to the pathogenesis of adhesive capsulitis8. A better understanding of these genetic links can guide future research on targeted non-operative treatments.
Shoulder surgery is a well-established risk factor for the development of adhesive capsulitis10,11. Specifically, breast cancer surgery is a risk factor unique to women, and survivors have a high rate of shoulder and upper extremity morbidity12. In a prospective study by Yang et al. of 271 women who underwent surgery for breast cancer, 10.3% and 7.7% had cumulative or current adhesive capsulitis, respectively, in the 13 to 18 month follow up period13. Another study found the prevalence of adhesive capsulitis to be 22% in the five years following breast cancer surgery. Mastectomy incurs additional risk compared to breast conserving surgery14. Subsequent reconstruction following mastectomy further increased the risk of developing adhesive capsulitis13,14. Given the high prevalence of adhesive capsulitis in this patient population, physicians should be vigilant and offer timely diagnosis and treatment.
Natural History and Management
The stages of adhesive capsulitis, originally proposed by Nevaisar et al. and further adapted by Redler et al. correlate arthroscopic pathology with clinical symptoms6,15. The three clinical stages progress from pain (Stage 1) to pain and stiffness (Stage 2) to primarily stiffness (Stage 3), and can help guide management. Adhesive capsulitis is often self-limited; however, a substantial portion of patients have some restriction of range of motion (ROM) at long term follow up4,16.
Nonoperative management consists of physical therapy, NSAIDs, oral corticosteroids, and intra-articular injections. Physical therapy has an unclear effect on long term disease course, and there is insufficient evidence favoring one form of physical therapy technique6,17. Anti- inflammatory medications may provide pain relief for clinical Stage 1 and 2 disease, but have not been shown to alter the disease course15,17. Hydrodilation, which involves the progressive dilation of the shoulder capsule, can be utilized, but there is conflicting evidence as to whether this provides additional benefit17. While capsular distention and steroid injections are effective conservative treatments, female sex is a negative modifier of effectiveness18.
Operative management is considered when non-operative treatment fails after a period of six months. Operative treatments include manipulation under anesthesia (MUA) and arthroscopic capsular release. These interventions can provide more rapid improvements in pain and ROM, but have not been shown to offer superior functional final outcomes17,19,20. In their retrospective study of predictors of surgery of adhesive capsulitis, Kingston et al. found that younger, white, and workers’ compensation patients were more likely to receive surgery. Sex, however, was not a predictor of surgical management21.
Multidirectional Instability
Hyperlaxity and Shoulder Instability
The diagnosis of multidirectional instability (MDI) in female athletes presents unique diagnostic and treatment challenges. MDI is differentiated from unidirectional instability by global laxity of the shoulder leading subluxation or dislocation inferiorly and in at least one other direction, anteriorly or posteriorly22. Females, often present with an atraumatic onset of symptoms, making the diagnosis more challenging23,24. Symptoms consist of shoulder fatigue, achiness, looseness and/or slipping, as well as transient sensory symptoms, often in the setting of shoulder hyperlaxity22,24. Hyperlaxity, however, is not necessarily pathologic; hyperlaxity must be symptomatic to be considered instability.
Female sex is correlated with both generalized and shoulder hyperlaxity. In their evaluation of 178 high school and collegiate athletes, McFarland et al. found a significantly higher rate of posterior and inferior shoulder laxity in females25. Borsa et al. assessed shoulder motion in normal, healthy adults using an arthrometer and found more anterior joint laxity in female shoulders26. Both authors also noted more generalized joint hypermobility in female patients25,26.
Sex Considerations in Diagnosis and Management
Female athletes may be especially susceptible to MDI, as they tend to favor sports requiring significant flexibility due to their baseline predisposition to joint hyperlaxity. Such sports include gymnastics, swimming, diving, and overhead throwing sports, which place repetitive stress on the shoulder. This repeated microtrauma can eventually lead to symptomatic laxity27.
Sex differences in the anatomy and biomechanics of the shoulder may contribute to the pathogenesis of certain shoulder conditions. Bonilla et al. found that male rat supraspinatus tendons exhibited a decreased dynamic modulus compared with female rat tendons, partially explaining the increased rate of acute rotator cuff tendon ruptures seen in young males compared with young females28. They also noted changes in the mechanical properties of rat tendons following estrogen withdrawal, suggesting a role of sex hormones in the pathogenesis of chronic supraspinatus tears in postmenopausal women28. In MDI, the sex differences in the pathophysiology are more likely related to the higher prevalence of hyperlaxity in female patients. Voyvhevk et al. found no difference in the composition of the shoulder capsule in males and females29. Kronberg et al., however, compared EMG activity of the shoulder stabilization musculature in patients with hyperlaxity with normal controls and found altered muscle activity in patients with hyperlaxity30.
Nonoperative treatment consists primarily of physical therapy aimed at strengthening dynamic shoulder stabilizers and targeting the direction of instability. Sex differences in shoulder biomechanics may contribute to response to physical therapy. The muscles acting out of phase or with increased activity in female patients with hyperlaxity are a target for physical therapy to restore normal mechanics30. Moreover, studies have demonstrated sex differences in the fatigue response of shoulder musculature, as females must work at higher intensities to generate similar workloads to men31,32. Physical therapy can yield satisfactory results, especially in the young, female population with hypermobility who will experience a decrease in instability symptoms as they age24,27,33,34.
In patients who fail conservative treatments, operative interventions are aimed at reducing capsular laxity while avoiding overtightening the joint. Surgical techniques include open capsular shift or arthroscopic capsulorrhaphy with concurrent treatment of any bony or soft tissue pathology22,27. Patients with significant anterior glenoid rim defects should be treated with an osteotomy and transfer of the coracoid process27,35,36. Female patients are more likely to require additional intraoperative rotator interval closure during pancapsular capsulorrhapy.
Despite this additional procedure, they are more likely to experience postoperative subluxations and have lower functional outcome scores, highlighting the challenge of treating this patient population23. Patients often have a postoperative reduction in shoulder ROM, which is an important consideration in the female athlete who relies on flexibility for success in her sport27. Preoperative counseling regarding the potential effect on athletic performance is encouraged.
Unidirectional Shoulder Instability
Disparities in Prevalence
While MDI is discussed in depth in the context of the female athlete, less attention has been paid to the sex-specific differences in traumatic anterior shoulder instability. Studies have demonstrated that the incidence of shoulder dislocation is 2 to 3 times higher in males than females. The majority of the literature reporting risk of recurrence for traumatic shoulder instability, as well as the outcomes following surgical intervention, are focused on male collision athletes – the cohort at highest risk for recurrence37-39. However, there are a number of female patients who suffer from traumatic anterior shoulder dislocations and recurrent instability40.
Leroux et al. studied all patients who underwent closed reduction between 2002 and 2010 for a first-time anterior glenohumeral dislocation40. While the authors found that young male patients had the highest incidence of primary anterior shoulder dislocation, females constituted over a quarter of the cohort (25.7%)40. When broken by age group (Figure 1), older females between the ages of 41 and 70 years old were at higher risk for requiring closed reduction than similarly aged males40. While this study confirms that young male patients have higher rates of primary and recurrent anterior shoulder dislocation than females, there are still a substantial number of female patients who sustain traumatic shoulder dislocations. Further research is necessary to determine optimal treatment for these patients.
Figure 1: Distribution of male and female cohort patients by age. The Y-axis depicts the percentage of patients, and the X-axis depicts age by year. As per legend, blue bars represent male patients, and red bars represent female patients.
Reproduced with permission from: Leroux T, Wasserstein D, Veillette C, et al. Epidemiology of primary anterior shoulder dislocation requiring closed reduction in Ontario, Canada. Am J Sports Med. 2014; 42(2): 442-50. DOI: 10.1177/0363546513510391
Sex Considerations in Operative Management
Treatment options for traumatic anterior shoulder instability include nonoperative management, arthroscopic or open Bankart repair, and Latarjet and Bristow procedures in the setting of significant glenoid bone loss. There may be sex-specific differences to consider when making these management decisions. Ljungquist et al. performed a cadaveric study examining male and female shoulder anatomy. They found that the absolute size of the glenoid (both width and length) was smaller in females than males and that the ratio of coracoid thickness to glenoid width was larger in male than in female specimens (Table 1)41. This provides interesting data about sex-specific differences in shoulder anatomy, assisting surgeons with preoperative planning.
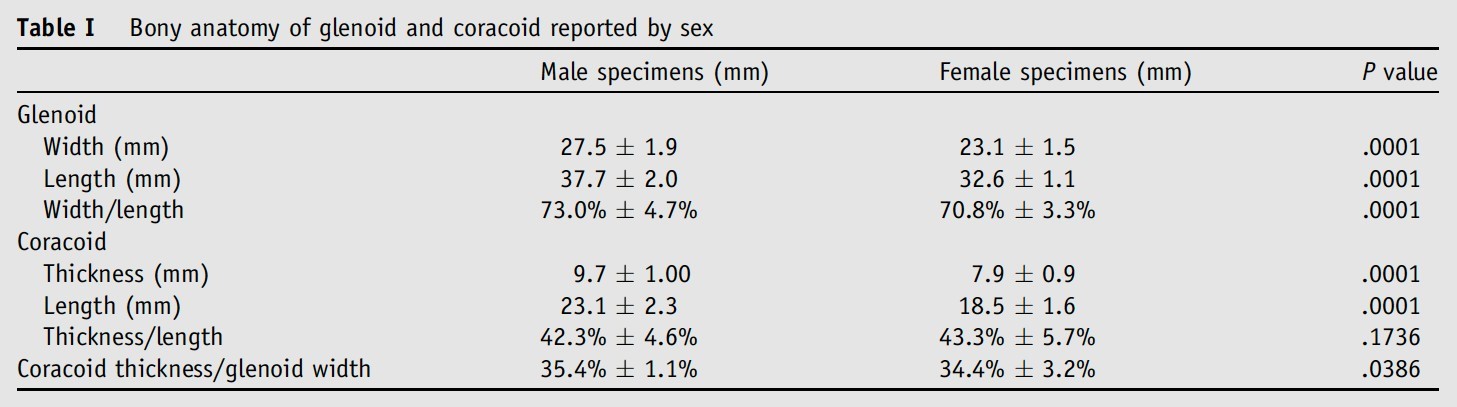
Reproduced with permission from: Ljungquist KL, Butler RB, Griesser MJ, et al. Prediction of coracoid thickness using a glenoid width-based model: implications for bone reconstruction procedures in chronic anterior shoulder instability. J Shoulder Elbow Surg. 2012; 21(6): 815-21. DOI: 10.1016/j.jse.2011.10.006.
Few studies have compared sex-specific differences in outcomes following surgical intervention for traumatic anterior shoulder instability, but female patients may have poorer outcomes following Bristow and Latarjet procedures. Hovelius et al. found that female patients undergoing Bankart repair or Bristow-Latarjet procedures had significantly worse DASH scores than male patients. There was also a trend toward worse outcomes in females with regard to WOSI, SSV, and SASF scores despite similar rates of recurrences42. Du Plessis et al. examined 29 female patients who had undergone a modified Latarjet procedure with at least one year of follow-up and reported a 13.8% reoperation rate with only 37.5% of these patients returning to sport43. While this study included patients who underwent the Latarjet procedure at a wide variety of ages (mean: 37.2 years, range: 20-66 years) and had other comorbidities (3 patients with epilepsy, 2 patients with alcohol abuse issues), the high complication rate and low rate of return to sport in this population is concerning. Given the paucity of literature available about traumatic anterior shoulder instability in the female athlete, additional studies are needed to better define risk factors and surgical outcomes in this population.
Conclusion
Adhesive capsulitis, multidirectional instability, and traumatic unidirectional shoulder instability are all important conditions to discuss in the context of female shoulder pathology. Women are more likely to get adhesive capsulitis than men, and it is an important cause of functional loss and impairment in middle-aged female populations. Females are much more likely to experience atraumatic shoulder instability than their male counterparts, likely due to higher rates of ligamentous laxity. Female athletes with atraumatic MDI can be challenging to diagnose and manage. Most studies that discuss traumatic anterior shoulder instability focus on the male cohort; however, women have been shown to have poorer surgical outcomes. Further research is needed to better understand and address this disparity.
Acknowledgement
No research grants or significant financial support were utilized for this study.
Conflict of Interest
The authors declare that neither they, their immediate families, nor any research foundation with which they are affiliated received any financial payments or other benefits from any commercial entity related to the subject of this article.
References
- Frank RM, Romeo AA, Bush-Joseph CA, et al. Injuries to the Female Athlete in 2017: Part I: General Considerations, Concussions, Stress Fractures, and the Female Athlete JBJS Rev. 2017; 5(10): e4. doi:10.2106/JBJS.RVW.17.00017
- Frank RM, Romeo AA, Bush-Joseph CA, et al. Injuries to the Female Athlete in 2017: Part II: Upper and Lower-Extremity Injuries. JBJS Rev. 2017; 5(10): e5. doi:10.2106/JBJS.RVW.17.00031
- Wang K, Ho V, Hunter-Smith DJ, et al. Risk factors in idiopathic adhesive capsulitis: a case control study. J Shoulder Elbow Surg. 2013; 22(7): e24-29. doi:10.1016/j.jse.2012.10.049
- Hand G, Carr A. Natural history and genetics of frozen shoulder a 1–20 year follow up of 273 patients. Orthopaedic Proceedings. 2005; 87-B(SUPP_II): 161-161. doi:10.1302/0301- 87BSUPP_II.0870161c
- Bulgen DY, Hazleman BL, Voak D. HLA-B27 and frozen shoulder. Lancet. 1976; 1(7968): 1042-1044. doi:10.1016/s0140-6736(76)92219-4
- Neviaser AS, Hannafin JA. Adhesive capsulitis: a review of current treatment. Am J Sports Med. 2010; 38(11): 2346-2356. doi:10.1177/0363546509348048
- Candela V, Giannicola G, Passaretti D, et al. Adhesive capsulitis of the shoulder: pain intensity and distribution. Musculoskelet Surg. 2017; 101(Suppl 2): 153-158. doi:10.1007/s12306-017-0488-6
- Prodromidis AD, Charalambous Is There a Genetic Predisposition to Frozen Shoulder? : A Systematic Review and Meta-Analysis. JBJS Rev. 2016; 4(2): e4. doi:10.2106/JBJS.RVW.O.00007
- Hakim AJ, Cherkas LF, Spector TD, et al. Genetic associations between frozen shoulder and tennis elbow: a female twin study. Rheumatology (Oxford). 2003; 42(6): 739- doi:10.1093/rheumatology/keg159
- Koorevaar RCT, Van’t Riet E, Ipskamp M, et al. Incidence and prognostic factors for postoperative frozen shoulder after shoulder surgery: a prospective cohort study. Arch Orthop Trauma Surg. 2017; 137(3): 293-301. doi:10.1007/s00402-016-2589-3
- Bailie DS, Llinas PJ, Ellenbecker TS. Cementless humeral resurfacing arthroplasty in active patients less than fifty-five years of age. J Bone Joint Surg Am. 2008; 90(1): 110-117. doi:10.2106/JBJS.F.01552
- Yang EJ, Park WB, Seo KS, et al. Longitudinal change of treatment- related upper limb dysfunction and its impact on late dysfunction in breast cancer survivors: a prospective cohort J Surg Oncol. 2010; 101(1): 84-91. doi:10.1002/jso.21435
- Yang S, Park DH, Ahn SH, et al. Prevalence and risk factors of adhesive capsulitis of the shoulder after breast cancer treatment. Support Care Cancer. 2017; 25(4): 1317-1322. doi:10.1007/s00520-016-3532-4
- Wong CJ, Tay MRJ, Aw HZ. Prevalence and Risk Factors of Adhesive Capsulitis in Asian Breast Cancer Patients Undergoing an Outpatient Community Cancer Rehabilitation Arch Phys Med Rehabil. 2021; 102(5): 843-848. doi:10.1016/j.apmr.2020.10.105
- Redler LH, Dennis ER. Treatment of Adhesive Capsulitis of the Shoulder. J Am Acad Orthop Surg. 2019; 27(12): e544-e554. doi:10.5435/JAAOS-D-17-00606
- Clarke GR, Willis LA, Fish WW, et al. Preliminary studies in measuring range of motion in normal and painful stiff shoulders. Rheumatol Rehabil. 1975; 14(1): 39-46. doi:10.1093/rheumatology/14.1.39
- Yip M, Francis AM, Roberts T, et al. Treatment of Adhesive Capsulitis of the Shoulder: A Critical Analysis Review. JBJS Rev. 2018; 6(6): e5. doi:10.2106/JBJS.RVW.17.00165
- Zhang J, Zhong S, Tan T, et al. Comparative Efficacy and Patient-Specific Moderating Factors of Nonsurgical Treatment Strategies for Frozen Shoulder: An Updated Systematic Review and Network Meta-analysis. Am J Sports Med. 2021; 49(6): 1669-1679. doi:10.1177/0363546520956293
- De Carli A, Vadalà A, Perugia D, et al. Shoulder adhesive capsulitis: manipulation and arthroscopic arthrolysis or intra-articular steroid injections? Int Orthop. 2012; 36(1): 101- doi:10.1007/s00264-011-1330-7
- Rangan A, Brealey SD, Keding A, et al. Management of adults with primary frozen shoulder in secondary care (UK FROST): a multicentre, pragmatic, three-arm, superiority randomised clinical trial. 2020; 396(10256): 977-989. doi:10.1016/S0140- 6736(20)31965-6
- Kingston K, Curry EJ, Galvin JW, et al. Shoulder adhesive capsulitis: epidemiology and predictors of surgery. J Shoulder Elbow Surg. 2018; 27(8): 1437-1443. doi:10.1016/j.jse.2018.04.004
- Cody E, Strickland S. Multidirectional Instability in the Female Athlete. Operative Techniques in Sports Medicine. 2014; (22): 34-43. doi:10.1053/j.otsm.2014.02.003
- Raynor MB, Horan MP, Greenspoon JA, et al. Outcomes After Arthroscopic Pancapsular Capsulorrhaphy With Suture Anchors for the Treatment of Multidirectional Glenohumeral Instability in Athletes. Am J Sports Med. 2016; 44(12): 3188- doi:10.1177/0363546516659644
- Brown GA, Tan JL, Kirkley A. The lax shoulder in females. Issues, answers, but many more Clin Orthop Relat Res. 2000; (372): 110-122.
- McFarland EG, Campbell G, McDowell Posterior shoulder laxity in asymptomatic athletes. Am J Sports Med. 1996; 24(4): 468-471. doi:10.1177/036354659602400410
- Borsa PA, Sauers EL, Herling Patterns of glenohumeral joint laxity and stiffness in healthy men and women. Med Sci Sports Exerc. 2000; 32(10): 1685-1690. doi:10.1097/00005768-200010000-00004
- Johnson SM, Robinson CM. Shoulder instability in patients with joint hyperlaxity. J Bone Joint Surg Am. 2010; 92(6): 1545-1557. doi:10.2106/JBJS.H.00078
- Bonilla KA, Pardes AM, Freedman BR, et al. Supraspinatus Tendons Have Different Mechanical Properties Across Sex. J Biomech Eng. 2019; 141(1): 0110021- doi:10.1115/1.4041321
- Voycheck CA, Rainis EJ, McMahon PJ, et al. Effects of region and sex on the mechanical properties of the glenohumeral capsule during uniaxial extension. J Appl Physiol (1985). 2010; 108(6): 1711-1718. doi:10.1152/japplphysiol.01175.2009
- Kronberg M, Broström LA, Németh Differences in shoulder muscle activity between patients with generalized joint laxity and normal controls. Clin Orthop Relat Res. 1991; (269): 181-192.
- Bouffard J, Yang C, Begon M, et al. Sex differences in kinematic adaptations to muscle fatigue induced by repetitive upper limb movements. Biol Sex Differ. 2018; 9(1): 17. doi:10.1186/s13293-018-0175-9
- Slopecki M, Messing K, Côté JN. Is sex a proxy for mechanical variables during an upper limb repetitive movement task? An investigation of the effects of sex and of anthropometric load on muscle Biol Sex Differ. 2020; 11(1): 60. doi:10.1186/s13293-020-00336-1
- Beasley L, Faryniarz DA, Hannafin Multidirectional instability of the shoulder in the female athlete. Clin Sports Med. 2000; 19(2): 331-349. doi:10.1016/s0278- 5919(05)70207-6
- Wright RW, Matava Treatment of multidirectional shoulder instability in the athlete. Operative Techniques in Sports Medicine. 2002; 10(1): 33-39. doi:10.1053/otsm.2002.29285
- Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007; 89(11): 1470-1477. doi:10.1302/0301-620X.89B11.18962
- Burkhart SS, De Beer JF, Barth JRH, et Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy. 2007; 23(10): 1033-1041. doi:10.1016/j.arthro.2007.08.009
- Hovelius L. Incidence of shoulder dislocation in Sweden. Clin Orthop Relat 1982; (166): 127-131.
- Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Am. 2010; 92(3): 542-549. doi:10.2106/JBJS.I.00450
- Owens BD, Agel J, Mountcastle SB, et al. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med. 2009; 37(9): 1750-1754. doi:10.1177/0363546509334591
- Leroux T, Wasserstein D, Veillette C, et Epidemiology of primary anterior shoulder dislocation requiring closed reduction in Ontario, Canada. Am J Sports Med. 2014; 42(2): 442-450. doi:10.1177/0363546513510391
- Ljungquist KL, Butler RB, Griesser MJ, et al. Prediction of coracoid thickness using a glenoid width-based model: implications for bone reconstruction procedures in chronic anterior shoulder instability. J Shoulder Elbow Surg. 2012; 21(6): 815-821. doi:10.1016/j.jse.2011.10.006
- Hovelius L, Vikerfors O, Olofsson A, et al. Bristow-Latarjet and Bankart: a comparative study of shoulder stabilization in 185 shoulders during a seventeen-year follow-up. J Shoulder Elbow Surg. 2011; 20(7): 1095-1101. doi:10.1016/j.jse.2011.02.005
- du Plessis JP, Dachs RP, Vrettos BC, et al. The modified Latarjet procedure in female patients: clinical outcomes and complications. J Shoulder Elbow Surg. 2018; 27(1): e9-e15. doi:10.1016/j.jse.2017.07.030
