A more accurate method to determine the magnification of radiographs when templating for hip arthroplasty?
Henry Magill1*, Mazin Ibrahim2, Foad Mohamed2, Samuel Grant3, Branavan Rudran4, Warwick Radford5
1Orthopaedic Registrar, Chelsea and Westminster Hospital, London, UK
2Orthopaedic Registrar, University College London Hospital, London, UK
3Orthopaedic Resident, University of Toronto, Toronto, Canada
4Orthopaedic Research Fellow, Chelsea and Westminster Hospital, London, UK
5Orthopaedic Consultant, Chelsea and Westminster Hospital, London, UK
Abstract
The use of digital templating for Total Hip Arthroplasty (THA) is now the standard approach for pre-operative planning. Digital templating holds potential to reduce operative time and post-op complications however, this often relies on imprecise assumptions. The relationship between the X-ray source, subject and detector alters the perceived magnification. We therefore determine if Body Mass Index (BMI) is positively correlated with true magnification and if a predictive model based these parameters exists. A single surgeon series (n=107) was included in this study. Two independent observers assessed both pre- and post-operative AP pelvis radiographs using TraumaCad™. Post-operative radiographs were assessed to calculate the true magnification by calibrating from a known femoral head prosthesis size. Finally, a scatter plot with regression was used to determine if a predictive model of magnification existed using the Body Mass Index. The mean pre-operative magnification using a scaling marker was 124.2 ± 8.90%. The mean post-operative magnification using a known femoral head prosthesis size (true magnification) was 123.7 ± 3.98%. Significant variability exists in pre-operative marker data. Regression modelling showed no significant correlation between BMI and true magnification (post-op magnification). This study’s suggests that the precision and reliability of the radiographic marker in daily practice is poor. Regression modelling showed no significant correlation between BMI and the true magnification factor. Therefore, a pre-op predictive model cannot be reliably used. The data from this study suggest that a fixed magnification factor of 124% remains the most reliable and accurate method.
Introduction
The use of digital templating for Total Hip Arthroplasty (THA) is conventional practice and is actively recommended. Precise templating of pre-operative radiographs holds potential to reduce operative time and post-op complications such as instability, leg length discrepancy, peri-prosthetic fracture and loosening1-4. Digital templating allows the surgeon to adjust the magnification, however, this often relies on imprecise assumptions and may result in an implant that is either too large or small.
The surgeon may be aided by the use of a radiopaque marker of known dimensions as a calibration tool to calculate the degree of magnification. In order for the method to produce reliable results, the marker must be in the same coronal plane as the hip joint and is often placed over the greater trochanter or in the perineum. Previous studies have shown that such markers give improved accuracy when compared to historical calliper measurements of the distance between anterior superior iliac spines5.
Many orthopaedic surgeons continue to template with an assumed magnification of 115-120%6-9. However, one study has reported an large inaccuracies when assuming a standard 120% magnification10. Recent studies by Archibeck and Franken et al. have also suggested that, when taking a fixed factor of 120% or 121% respectively, this remains more accurate than the use of a radiopaque marker11,12.
A post-operative radiograph assessing the implanted femoral head (of a known size) is the most precise technique to determine the true magnification, however, this is not available in the majority of cases when planning THA.
Aim
This study primarily evaluates the reliability of a standardised (25mm) pre-operative radiographic markers when estimating the true magnification when templating for THA.
The relationship between the X-ray source, subject and detector alters the perceived magnification [Figure 1]. Patients with larger amounts of soft-tissue between the hip joint and the detector may increase the distance between them and ultimately increase the magnification. We therefore hypothesise that Body Mass Index (BMI) may be positively correlated with magnification and that a predictive model based on BMI and true magnification exists.
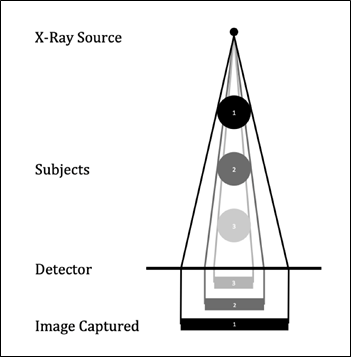
Figure 1: Schematic diagram showing how the relationship between X-ray source, subject and detector alters magnification.
Methods
We conducted a retrospective review including individuals who underwent primary hip arthroplasty between November 2018 and March 2019 by a single surgeon at a single institution. Our team assessed the pre- and post-operative radiographs of all individuals undergoing primary arthroplasty of a single hip for degenerative osteoarthritis. All radiographs were AP Pelvis radiographs in a supine position centred over the pubic symphysis. Radiographs were taken at a set standard distance of 120 cm from the X-Ray to detector.
All images were assessed using TraumaCad (BrainLAB, Munich, Germany) orthopaedic digital templating software. In order assess validity of the templating method, two independent and blinded observers analysed all radiographs.
The pre-operative films that used standard scaling marker (25 mm metallic sphere) were initially analysed (n=41, 38.3%). This included a radiopaque marker that should be placed at the coronal level of the acetabulum, using the greater trochanter as a surrogate marker.
The post-operative radiographs were then assessed to calculate the true magnification. The template software was used to calibrate from a known femoral head prosthesis size (28/32/36 mm) [Figure 2]. The femoral head component size was established from the operation record.
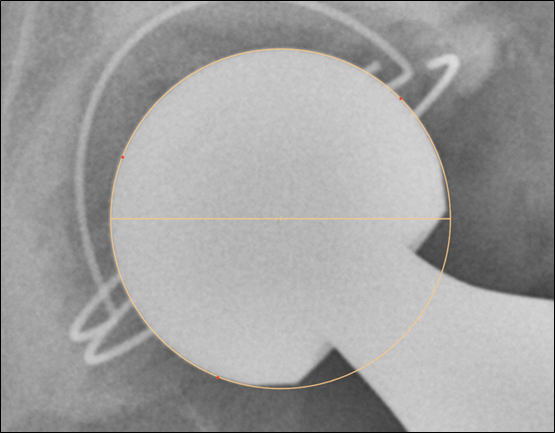
Figure 2: Demonstration of how digital templating tools are used to calibrate off a femoral head implant of a known size.
We decided not to assess the accuracy of pre-operative templating in predicting the actual size of component used; we appreciate the operating surgeon will have performed templating using the same radiographs and hence subject to bias.
Inter-observer variability was measured using paired-t tests for both pre-operative (scaling marker) and post-operative (known femoral head). Finally, we used a Scatter Plot with Regression to determine if a prediction model existed.
Results
This study identified a total of 107 (n=107) patients undergoing Total Hip Arthroplasty for degenerative osteoarthritis. Subjects underwent surgery between November 2018 and March 2019 with a mean age of 67.4 ± 11.5. 49 Males (45.8%) and 58 Females (54.2%) were included in the cohort. No patients were excluded. All implants used were hybrid with cemented stems. The mean pre-operative magnification assumption was 118%, this was used as standard practice for the single surgeon in this study.
There was an excellent agreement between both observers on radiographic measurements where the Pearson correlation coefficient was 0.894. Additionally, paired T-Testing revealed no significant difference between the first and the second observer (p = 0.8781).
The pre-operative magnification calculated using a scaling marker was used in only 41 of the 107 subjects (38.3%). The mean pre-operative magnification calculated was 124.2 ± 8.90%. The post-operative magnification using a known femoral head prosthesis size (true magnification) was calculated in all subjects in the study (n=107). The mean true magnification calculated was 123.7 ± 3.98%. A t-test was performed looking at pre-op magnification using the scaling marker and the corresponding pre-operative magnification. The results, based on 95% confidence levels, demonstrate no significant difference (p-value = 0.735) of the two means. However, significant variability of the pre-operative magnification (marker) data is noted (Var(X) = 79.2).
Regression modelling showed no significant correlation between BMI and true magnification (post-op magnification) and therefore excludes the use of a reliable pre-op predictive model [Figure 3].
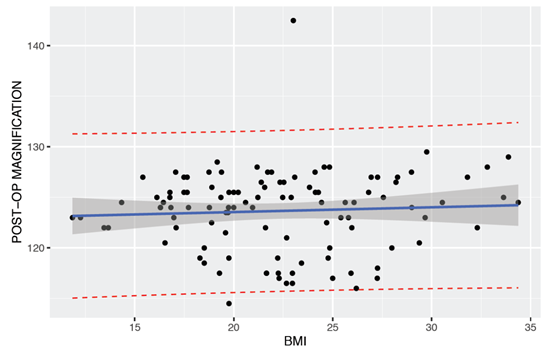
Figure 3: Scatter plot with regression line (solid line) showing the poor correlation between post-op true magnification and BMI. The dotted line indicates the 95% prediction limits and the inner grey area indicates 95% confidence limits.
Conclusion
Theoretically, if accurately placed, the pre-operative sizing marker should calibrate radiographs to a realistic true magnification8,13. The mean magnification from the sizing marker in this study was also 124%, however, this had significantly more variability than the mean (post-op) true magnification (SD ± 8.90%). This study also highlights that the precision of the radiographic marker is poor in this the observed population.
An assumed magnification factor of 118% will result in oversizing of the implanted components. The data from this study suggest that a fixed magnification factor of 124% remains the most reliable and accurate method.
Discussion
A fundamental step when templating a Total Hip Arthroplasty is to identify the true magnification of the radiographs. Accurate templating holds potential to reduce operative time and complications2-4. Many previous small studies have assumed or suggested the use of a magnification of 115-120%6-9. If incorrect magnification is used, the margin of error will depend on the increments in prosthesis size; one study has suggested that each magnification error of 2% corresponded to a different size of implant (ABG-II cementless)12.
A number of studies have implied that calibration from pre-operative sizing marker correlates to a much realistic true magnification8,13. However, such precise placement is not always possible in busy radiology departments. Reliable and consistent placement of the markers requires careful positioning by specifically trained radiographers. We suspect that in busy units this may not be possible due to the high turn-over of staff in the radiology department, the use of trainee radiographers and the fact that correct positioning of the marker high in the perineum may be uncomfortable and seen as socially unacceptable. Furthermore, where radiographs may show adequately placed markers, this may differ significantly from the correct coronal plane and remain too anterior or posterior. This study’s results therefore suggest that the precision of the radiographic marker in daily practice is poor and may be representative of many other orthopaedic departments’ results.
We appreciate that more extensive training and department guidelines could improve the positioning of the marker, and hence improve precision in predicting true magnification. However, this study has suggested the use of a simple and constant magnification factor may provide a more realistic and efficient solution. This technique allows simple and relatively accurate assumption of the true magnification without the requirement of radiographic markers. We do recommend that each institution that uses digital templating software carry out similar studies to self-assess validate a mean magnification factor; each department may use alternative image acquisition protocols from this study.
Acknowledgement
None
Conflict of Interest
Authors declare there is no conflict of interest in publishing the article.
References
- Descamps S, Livesey C, Learmonth ID. Determination of digitised radiograph magnification factors for pre-operative templating in hip prosthesis surgery. Skeletal Radiol. 2010.
- Petretta R, Strelzow J, Ohly NE, et al. Acetate Templating on Digital Images Is More Accurate Than Computer-based Templating for Total Hip Arthroplasty. Clin Orthop Relat Res. 2015.
- Eggli S, Pisan M, Müller ME. The value of preoperative planning for total hip arthroplasty. J Bone Jt Surg - Ser B. 1998.
- Marcucci M, Indelli PF, Latella L, et al. A multimodal approach in total hip arthroplasty preoperative templating. Skeletal Radiol. 2013.
- Wimsey S, Pickard R, Shaw G. Accurate scaling of digital radiographs of the pelvis. A prospective trial of two methods. J Bone Jt Surg - Ser B. 2006.
- White SP, Bainbridge J, Smith EJ. Assessment of magnification of digital pelvic radiographs in total hip arthroplasty using templating software. Ann R Coll Surg Engl. 2008.
- Brew CJ, Simpson PM, Whitehouse SL, et al. Scaling Digital Radiographs for Templating in Total Hip Arthroplasty Using Conventional Acetate Templates Independent of Calibration Markers. J Arthroplasty. 2012.
- Bayne CO, Krosin M, Barber TC. Evaluation of the Accuracy and Use of X-Ray Markers in Digital Templating for Total Hip Arthroplasty. J Arthroplasty. 2009.
- Heinert G, Hendricks J, Loeffler MD. Digital templating in hip replacement with and without radiological markers. J Bone Jt Surg - Ser B. 2009.
- Pickard R, Hiiggs D, Ward N. The accuracy of the PACS for pre-operative templating. Orthop Proc. 2018; 88(B).
- Archibeck MJ, Cummins T, Tripuraneni KR, et alet al. Inaccuracies in the Use of Magnification Markers in Digital Hip Radiographs. Clin Orthop Relat Res. 2016.
- Franken M, Grimm B, Heyligers I. A comparison of four systems for calibration when templating for total hip replacement with digital radiography. J Bone Jt Surg - Ser B. 2010.
- The B, Diercks RL, Stewart RE, et al. Digital correction of magnification in pelvic x rays for preoperative planning of hip joint replacements: Theoretical development and clinical results of a new protocol. Med Phys. 2005.
