30-Day Mortality Rates in Fractured Neck of Femur: Nottingham Hip Fracture Score vs Surgical Outcome Risk Tool
Michael Tang1, William Fowler1, Oday Al-Dadah1,2*
1Department of Trauma and Orthopaedic Surgery, South Tyneside District Hospital, Harton Lane, South Tyneside, United Kingdom
2Translational and Clinical Research Institute, Faculty of Medical Sciences, Newcastle University, Framlington Place, Newcastle-upon-Tyne, United Kingdom
Abstract
Objectives: The Nottingham hip fracture score (NHFS) and the Surgical outcome risk tool (SORT) are both validated scoring systems used to predict mortality rates in patient with Fractured neck of femur (FnF). The primary aim of this study was to compare the accuracy of the predicted 30-day mortality rates between NHFS and SORT in patients with FnF. The secondary aim was to investigate the influence of patient and surgical factors on 30-day mortality.
Methods: The NHFS and SORT score was collected from 212 patients admitted with FnF. Variables including hip fracture type, surgical procedure and peri-operative haemoglobin, gender and ASA grade were also collected and further analysed to assess their influence on 30-day mortality rates.
Results: Overall actual 30-day mortality rate for the study population was 11.3% (n=24). There was a significant difference between the mean predicted 30-day mortality for the NHFS (8.0%) and the SORT score (7.0%, p=0.006). The was no difference in mortality rates between the different fracture types (p=0.889). There was a significant difference in mortality rates when comparing surgical procedures (p=0.031). Patients who had a notable fall in haemoglobin peri-operatively had significantly higher mortality rates (p<0.001). Males had significantly higher mortality rates compared to females (20.0% vs 8.6% respectively, p=0.027). Higher ASA grades also had significantly higher mortality rates (p=0.003).
Conclusion: NHFS was found to be significantly more accurate at calculating 30-day mortality rates compared to the SORT score in patients with FnF. Surgical procedure and patient factors including gender, ASA grade and peri-operative haemoglobin also significantly influenced mortality rates but fracture type did not.
Introduction
Fractured neck of femur is the most common serious injury causing older patients to present to hospital1. In 2016, 65,000 people over the age of 65 presented to hospital with a fractured neck of femur costing the National Health Service (NHS) and social care £1 billon in the United Kingdom (UK)1. Mortality rates have improved in the past 50 years and vary dramatically based on co-morbidities, however a crude mortality rate of 6.7% was quoted for 20161.
Given the large number of patients and high mortality, being able to predict mortality rates is important for clinicians and provides valuable prognostic information for families. Two validated scoring systems for fractured neck of femur patients include the Nottingham Hip Fracture score (NHFS)2 and the Surgical Outcome Risk Tool (SORT)3. The clinical relevance of these scoring systems can be demonstrated on a patient level and to discuss with relatives the probable expectations of surviving the surgery. One can predict with some certainty that a patient with an NHFS score of 8 will likely have a worse outcome, than a patient with an NHFS score of 2.
The NHFS was initially developed in 2007 as a tool to predict 30-day mortality following hip fractures. The tool was then re-validated in 2012 across multiple centres and the scoring system subsequently updated to reflect the validated mortality rates. This tool uses multiple variables which are easily obtained as part of a routine hospital admission clerking to predict 30âday mortality.
The SORT is a similar tool which again uses variables which are easily acquired during a routine clerking to calculate 30-day mortality. The SORT score is an online web resource created by the collaborative effort between National confidential enquiry into patient outcome and death (NCEPOD) researchers and doctors in anaesthesia and intensive care medicine who are part of the Surgical Outcomes Research Centre (SOuRCe) team3.
Both tools give predicted mortality as a percentage at 30-days, however they give different results for the same patient.
The primary aim of this study was to compare the accuracy of the predicted 30-day mortality rates between NHFS and SORT in patients with fractured neck of femur. The secondary aim of this study was to investigate the influence of patient and surgical factors on 30-day mortality including type of hip fracture pattern, type of surgical procedure performed, gender, American Society of Anesthesiologists (ASA) physical status classification grade and peri-operative haemoglobin levels.
Materials and Methods
This is a retrospective cohort study (which did not require IRB / ethics committee approval) where all patients admitted to the department of Trauma and Orthopaedic surgery at a district general hospital with a diagnosis of fractured neck of femur between the dates of 1st January 2012 to 31st December 2012 were included. Data collected from the hospital records and patients notes included patient demographics, date of hospital admission, type of hip fracture and surgical procedure. The relevant information required to calculate both the NHFS (Table 1) and the SORT (Figure 1) scores were also collected. NHFS generates a final score as well as a mortality rate. SORT generates only a mortality rate.
Table 1: Nottingham Hip Fracture Score tool2
|
Variable |
Value |
score |
|
Age |
<66 |
0 |
|
|
66-85 |
3 |
|
|
>/=86 |
4 |
|
Sex |
Male |
1 |
|
Admission HB |
</=10g/dl |
1 |
|
MMSE* |
</=6 out of 10 |
1 |
|
Living in an institution |
yes |
1 |
|
Number of Co-morbidities |
>/= 2 |
1 |
|
Malignancy |
yes |
1 |
*Mini-Mental State Examination
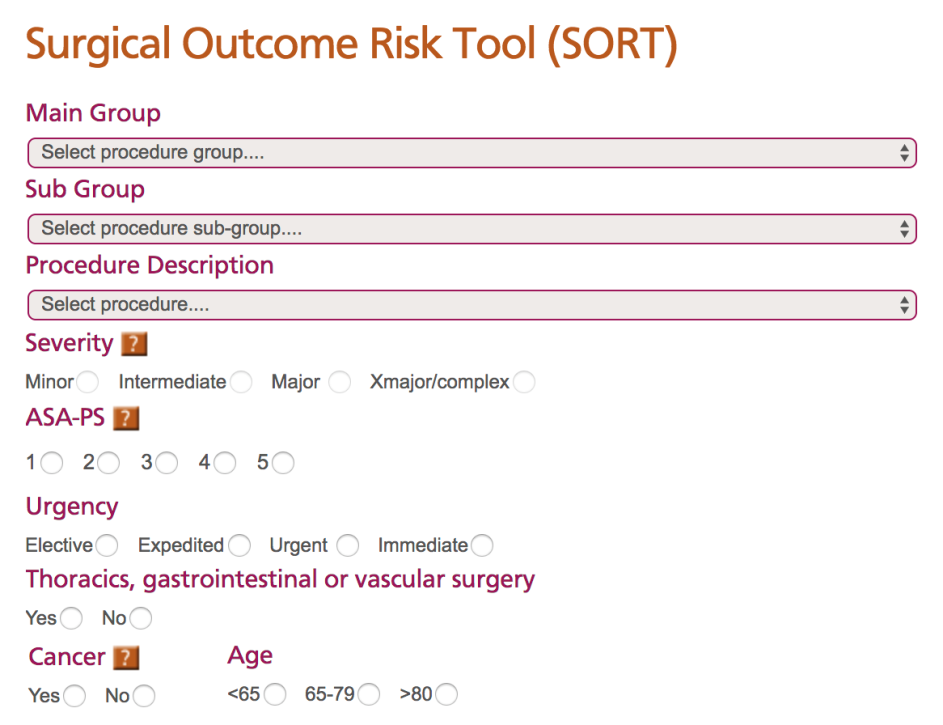
Figure 1: Surgical Outcome Risk Tool3
The overall actual 30-day mortality rate for the study population was calculated as was the predicted 30-day mortality rates based on NHFS and SORT. The results of which were then compared to assess their accuracy.
The variables of fracture pattern type (intra-capsular / extra-capsular), surgical procedure, ASA grade, gender and peri-operative haemoglobin were further evaluated to assess their influence on 30-day mortality rates.
Statistical Analysis
All continuous data sets (NHFS and SORT data) were assessed for normality of distribution by plotted histograms of the data which displayed a skewed distribution. This was verified by the Shapiro-Wilks test. The corresponding non-parametric statistical test for paired data (Wilcoxon Signed Rank Test) was used for this part of the data analysis. All binomial categorical data was analysed using the Pearson Chi-Square Test. The alpha significance level was set at 5% (p<0.05). Statistical analysis was performed using IBM SPSS version 24.0 (IBM Corp., Armonk, New York).
Results
A total of 212 patients were included in the study. Table 2 shows the patient demographics in the study.
Table 2: Patient Demographics
|
Demographic |
Number of patients |
|
Total number of patients (n) |
212 |
|
Male: Female |
50:162 |
|
Mean Age (yrs) (range) |
81.5 (46-103) |
|
Mean ASA* grade (range) |
2.8 (1-4) |
|
Intra-capsular: Extra-capsular fractures |
112:100 |
*American Society of Anesthesiologists physical status classification grade
The overall actual 30-day mortality rate for the study population was 11.3% (n=24).
Complete data was only available to calculate the NHFS for 156 patients. The mean NHFS score was 5.1 and the mean predicted 30-day morality rate was 8.0%. The actual (adjusted) 30-day mortality rate for this group (156 patients) was 7.7% (n=12). Of the remaining patients who had insufficient data to calculate the NHFS, 10 died within 30-days of hip surgery. Those who did have complete data (156 patients) to calculate the NHFS predicated 30-day mortality rate were then grouped according to their NHFS score and then compared to their actual 30-day mortality rates (Table 3). This shows that although overall the NHFS was good at predicting 30-day mortality, for each individual NHFS score group it was not as accurate, albeit in the extremes of each grouping the sample size was small.
Table 3: Comparison of NHFS predicted 30-day mortality and actual 30-day mortality (n=156)
|
NHFS Score |
Number of Patients |
Predicted 30-day mortality (%) |
Actual 30-day mortality (%) |
|
0 |
1 |
0.7 |
0 |
|
1 |
4 |
1.1 |
25 |
|
2 |
5 |
1.7 |
0 |
|
3 |
8 |
2.7 |
0 |
|
4 |
33 |
4.4 |
3.3 |
|
5 |
41 |
6.9 |
4.9 |
|
6 |
36 |
11 |
16.7 |
|
7 |
17 |
16 |
5.9 |
|
8 |
10 |
24 |
30 |
|
9 |
1 |
34 |
0 |
Complete data was available to calculate the SORT score for 205 patients. The mean predicted 30-day mortality rate for this group was 7.0%. The actual (adjusted) 30-day mortality rate for this group (205 patients) was 10.2% (n=21). Of the remaining patients who had insufficient data to calculate the SORT score, 3 died within 30-days of hip surgery.
There was a significant difference between the mean predicted 30-day mortality for the NHFS and the SORT score (Table 4).
Table 4: Comparison of NHFS vs SORT Predicted Mortality Rates
|
|
NHFS |
SORT |
p-value1 |
|
Mean Predicted Mortality (%) |
8.0 |
7.0 |
0.006* |
1Wilcoxon Signed Rank Test
*Statistically significant at <0.05
The comparison between fracture neck of femur pattern types (intra- vs extra-capsular) showed no difference in mortality rates (Table 5).
Table 5: Comparison of 30-day mortality and Type of Fracture
|
Type of Fracture |
Group Total (n) |
30-day Mortality (n) |
30-day Mortality Rate (%) |
p-value1 |
|
Intra-capsular |
112 |
13 |
11.6 |
0.889 |
|
Extra-capsular |
100 |
11 |
11.0 |
|
1Pearson Chi-Square Test
There was a significant difference in 30-day mortality rates among the different types of fracture fixation procedures and treatments (Table 6). Patients who had a total hip replacement (younger, healthier and more active patients) had a lower mortality rate, however conservatively managed patients (who were moribund and too unwell for surgery) had a significantly higher mortality rate. There were six patients who were treated conservatively, three who survived past 30-days. Of the three patients who survived 30-days, one had a fracture on the side of an above knee amputation, one died shortly after 30-days and the other was an impacted fractured who had been mobilising pain free.
Table 6: Comparison of 30-day mortality and Treatment Modality
|
Surgical Procedure |
Group Total (n) |
30-day Mortality (n) |
30-day Mortality Rate (%) |
p-value1 |
|
Hemi-arthroplasty |
89 |
11 |
8.1 |
0.031* |
|
THR2 |
19 |
0 |
0 |
|
|
Cannulated screws |
2 |
0 |
0 |
|
|
DHS3 |
78 |
9 |
11.5 |
|
|
IM4 Nail |
18 |
1 |
5.6 |
|
|
Conservative |
6 |
3 |
50.0 |
|
1Pearson Chi-Square Test
*Statistically significant at <0.05
2Total Hip Replacement
3Dynamic Hip Screw
4 Intra-Medullary
There was a significantly higher mortality rate in males compared to females (Table 7).
Table 7: Comparison of 30-day mortality and Gender
|
Gender |
Group Total (n) |
30-day Mortality (n) |
30-day Mortality Rate (%) |
p-value1 |
|
Male |
50 |
10 |
20.0 |
0.027* |
|
Female |
162 |
14 |
8.6 |
|
1Pearson Chi-Square Test
*Statistically significant at <0.05
The mortality rate significantly increased along with the ASA grade and was particularly high in ASA 4 patients (Table 8).
Table 8: Comparison of 30-day mortality and ASA
|
ASA |
Group Total (n) |
30-day Mortality (n) |
30-day Mortality Rate (%) |
p-value1 |
|
1 |
6 |
0 |
0 |
0.003* |
|
2 |
45 |
3 |
6.7 |
|
|
3 |
133 |
11 |
8.3 |
|
|
4 |
21 |
7 |
33.3 |
|
1Pearson Chi-Square Test
*Statistically significant at <0.05
Table 9 shows the comparison between the change in haemoglobin (comparing pre-operative haemoglobin levels with post-operative haemoglobin levels) and the effect on mortality. This revealed that a positive change (rise greater than 20 g/L) had the lowest mortality, in comparison to patients who had no significant change in haemoglobin levels and especially to patients who had a significant fall in their haemoglobin (reduction more than 20 g/L). Patients who demonstrated a rise in haemoglobin post-operatively was due to intra-operative blood transfusion which was done at the discretion of the anaesthetist. The general threshold for blood transfusion was a haemoglobin below 80g/l.
Table 9: Comparison of 30-day Mortality and the Change in Haemoglobin
|
Change in Haemoglobin (g/L) (pre-op vs post-op) |
Group Total (n) |
30-day Mortality (n) |
30-day Mortality Rate (%) |
p-value1
|
|
Negative change </=20 |
4 |
3 |
75.0 |
<0.001* |
|
Between -20 to +20 |
110 |
14 |
12.7 |
|
|
Positive change >/=20 |
102 |
7 |
6.9 |
|
1Pearson Chi-Square Test
*Statistically significant at <0.05
Discussion
The main findings of this study showed that the NHFS was more accurate at predicting 30-day mortality rates than the SORT score. Furthermore, fracture fixation and treatment modalities, gender, ASA grade and peri-operative haemoglobin levels all had a significant influence on mortality rates but fracture pattern type did not.
Both the NHFS and the SORT score can predict 30-day mortality in fractured neck of femur patients using clearly defined set of variables that are easy to gather8,9.
The NHFS was found to be more accurate at calculating crude 30-day mortality rates as compared to the SORT score in this study population. Possible reasons for this finding are that the former is a tool that has been specifically designed for calculating mortality in fractured neck of femur patients, rather than the SORT score which is a pan-surgical tool for calculating 30-day mortality rates for a large variety of surgical procedures. The latter is therefore a more generic tool.
Furthermore, the SORT score is less accurate as it uses more subjective variables, such as ASA and severity of operation6. The severity of operation is based on a pre-defined classification for private health insurance payments, rather than direct assessment of the physiological insult of surgery6. A further limitation of the SORT score is that the operations that they listed were not always complete and they suggested that the nearest equivalent could be used instead7. The NHFS also has subjective variables (i.e., number of co-morbidities)6. This field states that if the patient has 2 or more co-morbidities, they will get 1 point on the NHFS. It does not distinguish the severity of each co-morbidity. For example, a patient with osteoarthritis of the wrist and psoriasis would be given the same point score for that field as a patient with heart failure and myocardial infarction.
The main advantage of the SORT score is that there are fewer variables to collect, all of which are easily attainable. Protopapa et al.8 opted to omit data such as pre-operative haemoglobin levels and raised creatinine levels due to poor data collection from their initial study. As researchers wanted the SORT score to have greater generalizability, they wanted to develop a tool that was speedy and enabled collecting variables with ease as an important feature to retain. Protopapa et al.8 study collected a larger scale of data (5903 orthopaedic cases). Their study was however, not all fractured neck of femur patients, but a mixture of surgery of any urgency (immediate, urgent, expedited or elective) and required a planned overnight admission8.
Marufu et al.6 concluded that neither the NHFS nor the SORT score were particularly accurate for calculating 30-day mortality in fractured neck of femur patients after hip surgery. The SORT score was not more accurate than the NHFS and they also demonstrated that both have acceptable discriminatory ability, but after recalibration of both scores using adjusted co-efficients, found statistically similar predicted and observed 30-day mortality for the NHFS only6.
Although the NHFS did appear to accurately predict the overall mortality rate for this study’s group of patients, it did not appear to accurately predict the mortality for each individual NHFS score sub-group (0 to 9). A small sample size may well be the limiting factor for this however, given that a small number of patients were in each score sub-group.
It was not possible to calculate the NHFS in this study for a number of the patients due to the lack of documented mini-mental state examination (MMSE). It is difficult to state why the MMSE’s were not done in these cases. Some patients may have not been able to answer questions due to confusion (i.e., a score of 0) as well as the converse, the patient being so clearly orientated that the admitting doctor did not deem it necessary. However clearly this was a barrier in using the tool and indeed of retrospective studies overall which are heavily reliant on accurate note keeping of other professionals involved in the patient’s care.
In this study, the type of fracture pattern did not significantly affect the mortality rate. The logical explanation being that all surgical procedures for fracture neck of femurs represent a major operation. In Cornwall et al.5 study, they also showed that different fracture types do not have an effect on patient mortality rates, but it is rather each individual patient’s co-morbid factors that do have an effect on mortality. The results of the mortality rates compared to ASA grades in this study concur with the latter finding. The results of Kesmezacar et al.11, also showed there were no significant difference in mortality rates between inter-trochanteric and intra-capsular fractured neck of femur. However, Haentjens et al.12 demonstrated that inter-trochanteric fractures had an increased mortality at discharge from hospital and a year later on than compared to intra-capsular fractured neck of femur. Their study was a 1-year prospective study that focused on female patients only with no significant differences between the two groups with respect to median age (80 and 78 years, respectively), type and number of co-morbidities and pre-fracture residence at the time of injury12.
In this study, there was a significant difference in mortality rates between the different surgical procedures. Patients undergoing a total hip replacement had zero mortality as they represented younger, healthier and more active patients. Patients who were too medically unfit to undergo surgery (conservative treatment) had the highest mortality rates as they were moribund and unlikely to survive with or without surgery. Holt et al.10 found that internal fixation of an inter-trochanteric fracture produced a lower mortality rate than that of an uncemented hemi-arthroplasty.
In this study, there were more female patients which is in keeping with other studies in this field as females overall have a longer life expectancy. However, there was a significantly higher mortality rate in male patients. Kannegaard et al.13 showed a similar finding in their study but were unable to explain why this would be the case. There may be many factors which can account for the gender difference in mortality rates which may include co-morbidities, cognitive function, pre-morbid mobility status and living accommodation and intra-operative blood loss owing to larger dissections in proportionally larger patients.
In this study, we found a significant difference in mortality when evaluating the change of peri-operative haemoglobin levels. A positive haemoglobin change had the lowest mortality. Foss et al.4 have previously investigated the relationship between post-operative haemoglobin and mobility following surgery. Although their main aim was to show that anaemia impedes mobility post-operatively following hip surgery; their results also show that low post-operative haemoglobin is an independent risk factor for increased mortality following surgery. Willems et al.14 demonstrated that higher post-operative haemoglobin levels predict shorter length of hospital stay after hip fracture surgery in the elderly. A shorter stay in hospital is likely to mean a lower probability of contracting a hospital acquired infection or prolonged immobility leading to a thromboembolic event, thus, a decreased mortality rate. It should also be noted that the necessity of blood transfusion in itself is a known risk factor for post-operative complications and mortality.
All the post-operative haemoglobins collected were day one post-operative bloods. According to Nagra et al.15, the day 1 post-operative haemoglobin is an underestimation of the actual lowest value that is found on day 2. This is likely due to hidden blood loss, while there is still the active fracture haematoma and the blood loss consequent to intra-operate dissection16. In lieu of these findings, clinicians should not rely on day one post-operative blood results, but instead have more frequent haemoglobin checks should be performed on post-operative patients to prevent severe anaemia complicating patient’s stay in hospital.
Suggestions for further study include investigating the relationship between haemoglobin levels and the use of blood transfusions, particularly looking into the effect on mortality rates, but also on the effect of length of hospital stay and need for prolonged rehabilitation.
It was noted that the overall mortality rate (11.3%) in this study was higher than that of the data collected by Moppet et al. (6.6%) upon which the modified NHFS is based2. The Modified Nottingham Hip Fracture Score results in the latter study was a mean NHFS of 4.5 as compared to our study population with a mean of 5.1 (Respective medians of 4 and 5). This illustrates that the patient population within our geographic location (North-East England, UK) presenting to our institution have more risk factors (i.e. more co-morbidities) which in turn will have a profound effect on mortality rates. The distribution of our patients NHFS score in comparison to those in the Moppet et al.2 study is shown in Table 10.
Table 10: NHFS Comparison between current study group and modified NHFS publication2
|
NHFS Score |
Proportion of total patients in sample (%) |
Proportion in modified NHFS data (%) |
|
0 |
0.6 |
2 |
|
1 |
2.6 |
1 |
|
2 |
3.2 |
1 |
|
3 |
5.1 |
21 |
|
4 |
21.2 |
27 |
|
5 |
26.3 |
25 |
|
6 |
23.1 |
16 |
|
7 |
11 |
6 |
|
8 |
6.4 |
1 |
|
9 |
0.6 |
0.03 |
The main limitation of this study was that many patients were missing data required to calculate their NHFS. In total, 56 patients had data missing regarding their MMSE specifically which consequently reduced the sample size that can have their NHFS feasibly calculated. This has since been rectified in our department with the implementation of a proforma that is completed for all patients with a fractured neck of femur which mandates that MMSE must be completed by all doctors upon hospital admission. There was also some data missing due to lost paper work but this is a general limitation of all retrospective studies. Another limitation is with calculating the SORT scores as the tool ranks all surgical operations as ‘major-complex’ with the exception of cannulated screws which it ranks as only ‘Major’, despite all operations, from a surgical prospective, being equally complex, sizable and physiologically imposing on these elderly frail patients. This may mean that fundamentally the SORT score under-ranks mortality for patients undergoing cannulated screw fixation, and may affect the results in this respect. Surgical delay of greater than 48 hours is a known risk factor for increased mortality rate following hip fractures. It is recommended that future studies also include an evaluation of this data too.
Conclusion
This study has shown that NHFS was significantly more accurate at calculating 30-day mortality rates compared to the SORT score in patients with fractured neck of femur. The former is a more specific tool for this purpose and the latter is a more generic tool. Surgical procedure and patient factors including gender, ASA grade and peri-operative haemoglobin also significantly influenced mortality rates but fracture type did not.
References
- Royal College of Physicians. National Hip Fracture Database annual report 2017. London: RCP, 2017.
- Moppett IK, Parker M, Griffiths R, et al. Nottingham Hip Fracture Score: longitudinal and multi-centre assessment. Br J Anaesth. 2012; 109(4): 546-50. https://doi.org/10.1093/bja/aes187
- NCEPOD, Source. (Available from) (accessed April 2018) Surgical outcome risk tool (SORT); 2015. http://www.sortsurgery.com/
- Foss NB, Kristensen MT, Kehlet H. Anaemia impedes functional mobility after hip fracture surgery. Age Ageing. 2008; 37(2): 173-8. https://doi.org/10.1093/ageing/afm161
- Cornwall R, Gilbert MS, Koval KJ, et al. Functional Outcomes and Mortality Vary among Different Types of Hip Fractures: A Function of Patient Characteristics. Clinical orthopaedics and related research. 2004; (425): 64-71. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1455528/
- Marufu TC, White SM, Griffiths R, et al. Prediction of 30âday mortality after hip fracture surgery by the Nottingham Hip Fracture Score and the Surgical Outcome Risk Tool. Anaesthesia. 2016; 71(5): 515-21. doi:1111/anae.13418
- Protopapa KL. Is there a place for the Surgical Outcome Risk Tool app in routine clinical practice? Br J Hosp Med (Lond). 2016; 77(11): 612-613. Available from: http://www.ncepod.org.uk/pdf/publications/SORTeditorialInBJHM_Nov_2016.pdf
- Protopapa KL, Simpson JC, Smith NC, et al. Development and validation of the Surgical Outcome Risk Tool (SORT). Br J Surg. 2014; 101(13): 1774-83. doi:1002/bjs.9638
- Kau CY, Kwek EB. Can preoperative scoring systems be applied to Asian hip fracture populations? Validation of the Nottingham Hip Fracture Score (NHFS) and identification of preoperative risk factors in hip fractures. Annals of the Academy of Medicine Singapore. 2014; 43: 448–53.
- Holt EM, Evans RA, Hindley CJ, et al. 1000 femoral neck fractures: the effect of pre-injury mobility and surgical experience on outcome. International Journal of The Care of The Injured, 1994; 25(2): 91-5.
- Kesmezacar H, Ayhan E, Unlu MC, et al. Predictors of mortality in elderly patients with an intertrochanteric or a femoral neck fracture. J Trauma. 2010; 68(1): 153-158.
- Haentjens P, Autier P, Barette M, et al. Survival and functional outcome according to hip fracture type: A one-year prospective cohort study in elderly women with an intertrochanteric or femoral neck fracture. Bone. 2007; 41(6): 958-64. 10.1016/j.bone.2007.08.026.
- Kannegaard PN, van der Mark S, Eiken P, et al. Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing. 2010; 39(2): 203-9.
- Willems JM, de Craen AJ, Nelissen RG, et al. Hemoglobin predicts length of hospital stay after hip fracture surgery in older patients. Maturitas. 2012; 72(3): 225-8.
- Nagra NS, van Popta D, Whiteside S, et al. An analysis of postoperative hemoglobin levels in patients with a fractured neck of femur, Acta Orthopaedica et Traumatologica Turcica. 2016; 50(5): 507-513.
- Foss NB, Kehlet H. Hidden blood loss after surgery for hip fracture. J Bone Joint Surg Br. 2006; 88(8): 1053-9.
